The use of botanical remedies to alleviate the symptoms of digestive tract inflammation, specifically targeting both the stomach and intestines, represents a traditional approach to addressing this common ailment. This encompasses employing plant-derived substances to manage discomfort, reduce inflammation, and potentially expedite recovery from the condition.
Historically, various cultures have relied on plant-based therapies for managing such conditions. The perceived advantages often include accessibility, affordability, and a perceived lower risk of adverse effects compared to conventional pharmaceutical interventions. The appeal lies in the potential to address symptoms in a natural and holistic manner.
The efficacy and safety of employing such remedies are topics of ongoing investigation. The following sections will delve into specific botanical options, their purported mechanisms of action, and the current state of evidence supporting their application in managing the aforementioned condition.
Considerations for Addressing Digestive Inflammation with Botanicals
The following points offer guidance when exploring plant-derived substances for managing inflammation affecting the digestive system.
Tip 1: Hydration is Paramount: Maintaining adequate fluid intake is crucial. Dehydration can exacerbate symptoms; therefore, consistent consumption of water, herbal teas, or electrolyte-rich solutions is advised.
Tip 2: Identify Potential Triggers: Certain foods or substances may intensify symptoms. Keeping a detailed log of dietary intake can assist in identifying and subsequently eliminating such triggers.
Tip 3: Embrace Gentle Herbs: Ginger, chamomile, and peppermint have demonstrated potential in alleviating nausea, reducing inflammation, and soothing the digestive tract. These can be consumed as teas or in encapsulated form.
Tip 4: Probiotic Supplementation: Introducing beneficial bacteria to the gut microbiome may aid in restoring digestive balance. Select a probiotic supplement with strains known to support gastrointestinal health.
Tip 5: Dietary Adjustments: Adhering to a bland diet, consisting of easily digestible foods such as bananas, rice, applesauce, and toast (the BRAT diet), can minimize digestive strain during the acute phase.
Tip 6: Gradual Reintroduction of Foods: Once symptoms begin to subside, gradually reintroduce foods to assess tolerance. Start with small portions of easily digestible options.
Tip 7: Prioritize Rest: Adequate rest and sleep are essential for supporting the body’s natural healing processes. Minimize physical exertion during the acute phase.
These considerations aim to provide a structured approach to symptom management. Individual responses to botanical and dietary interventions may vary.
The subsequent sections will elaborate on specific herbal options and their application within a comprehensive management strategy.
1. Anti-inflammatory properties
The inflammatory response within the gastrointestinal tract is a central characteristic of gastroenteritis, regardless of its etiology (viral, bacterial, parasitic, or dietary). The cardinal signs of inflammation redness, swelling, heat, and pain manifest as abdominal cramping, diarrhea, and vomiting. Therefore, interventions aimed at mitigating this inflammatory cascade are logically incorporated into management strategies. Botanicals possessing inherent anti-inflammatory properties represent one such approach. The underlying principle is that by modulating the inflammatory response, the severity of symptoms and the duration of the illness can be reduced.
Herbs such as ginger ( Zingiber officinale ) and chamomile ( Matricaria chamomilla) exemplify this concept. Ginger contains gingerols, compounds demonstrated to inhibit the production of pro-inflammatory cytokines, thereby lessening the inflammatory burden. Similarly, chamomile contains apigenin, a flavonoid with documented anti-inflammatory effects. These botanicals do not act as direct antiviral or antibacterial agents (in most cases); rather, they address the secondary inflammatory response triggered by the pathogen or irritant. A practical example is the use of ginger tea to alleviate nausea and abdominal discomfort associated with viral gastroenteritis; while it doesn’t eradicate the virus, it can provide symptomatic relief by modulating inflammation.
Understanding the anti-inflammatory potential of botanicals is crucial for informed decision-making regarding their use. While these remedies are generally considered safe, it is essential to recognize that they do not replace conventional medical care in severe cases. Furthermore, the specific compounds responsible for anti-inflammatory activity vary between herbs, and their efficacy depends on factors such as dosage and individual patient characteristics. Integrating such botanical options into a comprehensive management plan, alongside rehydration and dietary modifications, represents a rational approach to mitigating the inflammatory component of gastroenteritis. Further rigorous clinical research is needed to fully elucidate the optimal application and efficacy of these agents.
2. Antimicrobial action
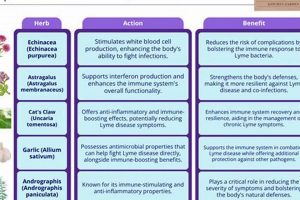
Antimicrobial action constitutes a critical, albeit sometimes overstated, aspect of botanical interventions for gastroenteritis. While not all instances of gastroenteritis stem from microbial infections, those that do may potentially benefit from herbs exhibiting antimicrobial properties. It is essential to differentiate between direct antimicrobial effects and the modulation of the host’s immune response.
- Direct Pathogen Inhibition
Certain herbs contain compounds capable of directly inhibiting the growth or replication of common gastroenteritis-causing pathogens. For instance, garlic ( Allium sativum) contains allicin, which has demonstrated in vitro activity against bacteria like Escherichia coli and Salmonella. Similarly, oregano oil, rich in carvacrol, possesses broad-spectrum antimicrobial properties. The implication here is that these herbs, if consumed in sufficient concentrations, may potentially contribute to reducing the pathogen load within the gastrointestinal tract.
- Immune System Modulation
Rather than directly targeting the pathogen, some herbs bolster the host’s immune defenses, thereby facilitating pathogen clearance. Echinacea ( Echinacea purpurea), while primarily known for its immunostimulatory effects on the respiratory system, may indirectly support the gut’s immune response. This is particularly relevant in cases where the infection is viral, as direct antiviral herbal agents are limited. By enhancing immune function, the body becomes better equipped to combat the infection.
- Selective Antimicrobial Activity
The gut microbiota comprises a complex ecosystem of both beneficial and potentially harmful microorganisms. Broad-spectrum antibiotics, while effective against pathogens, can disrupt this delicate balance, leading to dysbiosis. Herbs with selective antimicrobial activity, targeting specific pathogens while sparing beneficial bacteria, may offer an advantage. Berberine, found in herbs like goldenseal ( Hydrastis canadensis) and barberry ( Berberis vulgaris), exhibits such selective activity, inhibiting certain pathogens without significantly impacting the overall gut microbiome.
- Bioavailability Considerations
The effectiveness of antimicrobial herbs hinges on their bioavailability within the gastrointestinal tract. Many compounds are poorly absorbed, meaning that only a fraction reaches the site of infection. Factors such as the form of administration (e.g., capsules, teas, tinctures) and the presence of other substances in the gut can influence bioavailability. Therefore, even if an herb demonstrates potent antimicrobial activity in vitro, its in vivo efficacy may be limited by poor absorption.
The role of antimicrobial action in botanical gastroenteritis management is nuanced. While certain herbs possess demonstrable antimicrobial properties, their effectiveness depends on factors such as the specific pathogen involved, the herb’s bioavailability, and the overall health of the host. Moreover, it is crucial to distinguish between direct pathogen inhibition and immune modulation. Employing such herbs judiciously, alongside other supportive measures like rehydration and dietary modifications, can potentially contribute to a more comprehensive approach to managing infectious gastroenteritis. Further research is necessary to clarify the optimal application and efficacy of specific antimicrobial herbs.
3. Soothing demulcents
Demulcents, characterized by their mucilaginous properties, represent a specific category of herbal remedies employed in gastroenteritis to alleviate irritation and inflammation within the gastrointestinal tract. Their relevance stems from their ability to form a protective layer over inflamed mucosal surfaces, reducing direct contact with irritants and gastric acids.
- Mechanism of Action
Demulcents exert their effects by creating a viscous coating that physically shields the lining of the esophagus, stomach, and intestines. This barrier minimizes exposure to acidic gastric contents, digestive enzymes, and other potentially irritating substances present during gastroenteritis. The reduction in direct irritation contributes to the alleviation of pain, nausea, and the urge to vomit.
- Examples of Demulcent Herbs
Slippery elm ( Ulmus rubra) is a prime example, containing a high mucilage content that expands when mixed with water, forming a gel-like substance. Marshmallow root ( Althaea officinalis) and licorice root ( Glycyrrhiza glabra, used cautiously due to potential blood pressure effects) also possess demulcent properties. These herbs are typically administered as teas, powders mixed with water, or in encapsulated form.
- Application in Gastroenteritis
In cases of gastroenteritis characterized by heartburn, abdominal cramping, or frequent vomiting, demulcents can provide symptomatic relief by reducing irritation of the gastrointestinal mucosa. They are often used in conjunction with other herbal and conventional therapies, such as antiemetics and rehydration solutions. The protective coating they provide allows the inflamed tissues to heal more effectively.
- Considerations and Cautions
While generally considered safe, demulcents can potentially interfere with the absorption of certain medications if taken concurrently. It is advisable to administer demulcents at least one hour apart from other oral medications. Individuals with known allergies to plants within the same family as the specific demulcent herb should exercise caution. As with any herbal remedy, consulting a healthcare professional is recommended before use, particularly for individuals with pre-existing medical conditions or those taking prescription medications.
The incorporation of soothing demulcents into a holistic approach to gastroenteritis management acknowledges the importance of protecting and supporting the gastrointestinal lining. Their ability to reduce irritation and promote healing underscores their value as a complementary therapy, particularly in mitigating the discomfort associated with the condition.
4. Gut microbiome support
Gastroenteritis, irrespective of its etiology, often precipitates a disruption of the gut microbiome, the complex community of microorganisms residing within the gastrointestinal tract. This dysbiosis, characterized by a reduction in beneficial bacteria and a potential proliferation of pathogenic organisms, can exacerbate symptoms and prolong recovery. Consequently, interventions aimed at restoring and supporting a healthy gut microbiome represent a logical and integral component of a comprehensive approach to managing gastroenteritis.
Botanical remedies can play a multifaceted role in supporting gut microbiome health during and after gastroenteritis. Certain herbs, such as those containing prebiotics (non-digestible fibers that nourish beneficial bacteria), can selectively promote the growth of advantageous microbial species. For example, dandelion root ( Taraxacum officinale) and chicory root ( Cichorium intybus) are rich in inulin, a prebiotic fiber that supports the growth of Bifidobacteria. Furthermore, some herbs possess antimicrobial properties that can selectively target pathogenic bacteria, thereby reducing their impact on the gut microbiome. Berberine-containing herbs, like goldenseal, exemplify this selective antimicrobial activity. The strategic use of such botanicals can help to re-establish a balanced gut microbiome following the disruption caused by gastroenteritis. Practical examples include the consumption of herbal teas containing prebiotic herbs and the incorporation of fermented foods, like sauerkraut (if tolerated), alongside appropriate herbal remedies to foster a diverse and resilient gut microbiome.
The importance of gut microbiome support in gastroenteritis management extends beyond symptom alleviation. A balanced gut microbiome is crucial for optimal immune function, nutrient absorption, and the prevention of recurrent infections. By incorporating targeted botanical interventions to support the gut microbiome, individuals can potentially expedite recovery, reduce the risk of complications, and promote long-term gastrointestinal health. However, it is crucial to acknowledge the complexity of the gut microbiome and the potential for individual variability in response to herbal interventions. Careful consideration of individual health status, potential interactions with other medications, and the specific characteristics of the botanical remedy are essential for safe and effective application. Ongoing research continues to elucidate the intricate interplay between botanicals and the gut microbiome, paving the way for more targeted and personalized approaches to gastroenteritis management.
5. Symptom management
Symptom management forms a cornerstone in addressing gastroenteritis. The utilization of botanical remedies frequently centers on alleviating the most distressing manifestations of the condition, providing a degree of comfort and facilitating the body’s natural healing processes. This approach prioritizes targeted relief of specific symptoms.
- Nausea and Vomiting Alleviation
Specific botanicals exhibit antiemetic properties, aiding in the reduction of nausea and the suppression of vomiting. Ginger ( Zingiber officinale), for example, contains gingerols which modulate gastric motility and reduce the sensation of nausea. Peppermint ( Mentha piperita) can also soothe the stomach and reduce the urge to vomit. These are often consumed as teas or in encapsulated forms to provide prompt relief.
- Diarrhea Control
Certain herbs possess astringent qualities, which can help to reduce the frequency and liquidity of bowel movements. Agrimony ( Agrimonia eupatoria) and Blackberry leaf ( Rubus fruticosus) are traditionally employed for this purpose. These herbs contain tannins that constrict tissues and reduce fluid secretion into the intestines. Careful use is essential to avoid excessive constipation.
- Abdominal Cramping and Pain Reduction
Antispasmodic herbs can help to ease abdominal cramping associated with gastroenteritis. Chamomile ( Matricaria chamomilla) and Peppermint ( Mentha piperita) exert antispasmodic effects, relaxing the smooth muscles of the gastrointestinal tract. This reduction in muscle spasms contributes to pain relief and reduced abdominal discomfort.
- Dehydration Mitigation
While not directly addressing the underlying cause of gastroenteritis, certain herbal teas can contribute to rehydration and electrolyte replenishment. Electrolyte-rich herbal infusions can help to restore fluid balance, particularly in cases of significant fluid loss due to vomiting and diarrhea. However, they should not be considered a replacement for oral rehydration solutions in severe cases.
The application of botanicals for symptom management in gastroenteritis aims to provide targeted relief and support the body’s natural healing processes. While these remedies can be beneficial, they should not be considered a substitute for conventional medical care, especially in severe cases or for vulnerable populations. Symptomatic relief should ideally complement strategies addressing the underlying cause of the illness.
6. Hydration maintenance
Hydration maintenance is critically intertwined with the successful application of botanical therapies for gastroenteritis. Gastroenteritis, characterized by vomiting and diarrhea, invariably leads to fluid and electrolyte losses, creating a state of dehydration. Dehydration exacerbates the symptoms of gastroenteritis, impairs physiological function, and can, in severe cases, become life-threatening. Consequently, any therapeutic approach to gastroenteritis, including botanical interventions, must prioritize adequate rehydration.
Botanical remedies for gastroenteritis are frequently administered as teas or infusions. These preparations inherently contribute to fluid intake, thereby partially addressing the dehydration associated with the illness. Specific herbal teas, such as chamomile or ginger, offer dual benefits: they provide hydration and deliver the therapeutic properties of the herb. For instance, a mild chamomile tea not only replenishes fluids lost through vomiting or diarrhea but also leverages the anti-inflammatory and antispasmodic effects of chamomile to soothe the gastrointestinal tract. Similarly, ginger tea provides fluid while simultaneously mitigating nausea. Electrolyte imbalances, another consequence of fluid loss, can be addressed through herbal teas formulated to include small amounts of salt and sugar, mimicking basic oral rehydration solutions. However, it is crucial to acknowledge that herbal teas alone may be insufficient to address severe dehydration, necessitating the use of commercially available oral rehydration solutions or, in critical cases, intravenous fluid administration. The practical significance lies in the understanding that botanical remedies for gastroenteritis should always be integrated within a comprehensive rehydration strategy, tailoring the approach to the severity of fluid loss.
In summary, hydration maintenance is not merely an adjunct to botanical therapies for gastroenteritis but a foundational element. The benefits of herbal remedies are significantly diminished if adequate hydration is not maintained. While herbal teas can contribute to fluid intake and deliver therapeutic compounds, they should be considered as part of a broader rehydration plan, supplemented by oral rehydration solutions when necessary. Challenges remain in accurately assessing the degree of dehydration and ensuring consistent fluid intake, particularly in vulnerable populations such as infants and the elderly. However, prioritizing hydration maintenance alongside botanical interventions represents a rational and evidence-based approach to managing gastroenteritis.
7. Traditional usage
The connection between traditional usage and gastroenteritis herbal treatment is fundamental, as it represents the historical basis upon which many contemporary applications are built. Traditional usage embodies accumulated knowledge, passed down through generations, regarding the selection, preparation, and administration of botanicals for managing digestive ailments. This knowledge frequently arises from empirical observation: noticing the effects of certain plants on individuals experiencing symptoms like diarrhea, vomiting, or abdominal pain. The importance lies in the recognition that traditional systems of medicine provide a rich repository of potential therapeutic agents, some of which may possess efficacy supported by modern scientific investigation. For example, the long-standing use of ginger in numerous cultures to alleviate nausea is mirrored by contemporary research demonstrating its antiemetic properties. Similarly, the application of chamomile for soothing digestive upset aligns with current understanding of its anti-inflammatory and antispasmodic effects.
Further analysis reveals that traditional practices are not static; they evolve over time, influenced by cultural exchange and the integration of new knowledge. The preparation methods, dosages, and combinations of herbs used in traditional gastroenteritis treatments often reflect a nuanced understanding of plant pharmacology and the individual patient’s constitution. Practical application requires careful consideration of the specific herbal traditions, as variations exist across different geographic regions and cultural groups. For instance, the Ayurvedic system of medicine in India utilizes a distinct set of herbs and treatment protocols compared to Traditional Chinese Medicine or traditional European herbalism. Understanding these nuances is critical for ensuring the safe and effective application of herbal remedies. Real-life examples, such as the continued use of specific herbal formulas for diarrhea in Traditional Chinese Medicine clinics, underscore the relevance of traditional knowledge in contemporary healthcare.
In conclusion, the insights gained from studying traditional usage are crucial for informing modern gastroenteritis herbal treatment. While not all traditional remedies will withstand rigorous scientific scrutiny, the accumulated experience embedded within these practices provides a valuable starting point for identifying potentially effective botanical agents. Challenges remain in translating traditional knowledge into standardized, evidence-based treatments. However, by combining the wisdom of traditional usage with the rigor of modern science, a more comprehensive and effective approach to managing gastroenteritis can be developed. This approach acknowledges the importance of historical context while emphasizing the need for ongoing research and critical evaluation.
Frequently Asked Questions Regarding Botanical Approaches to Gastroenteritis
This section addresses prevalent inquiries concerning the employment of botanical remedies in the management of gastroenteritis. The information presented is intended for educational purposes and does not constitute medical advice. Consultation with a qualified healthcare professional is essential before initiating any treatment regimen.
Question 1: Are botanical treatments a substitute for medical care in gastroenteritis?
Botanical treatments are not a substitute for conventional medical care, particularly in cases of severe dehydration, persistent vomiting, high fever, or bloody stools. The primary focus in gastroenteritis management is rehydration and electrolyte balance, which may require medical intervention.
Question 2: What specific herbs are commonly used for gastroenteritis?
Commonly cited herbs include ginger (for nausea), chamomile (for inflammation and cramping), peppermint (for cramping and nausea), and slippery elm (for soothing irritated tissues). However, individual responses may vary, and not all herbs are suitable for all individuals.
Question 3: How are herbal remedies for gastroenteritis typically administered?
Herbal remedies are frequently administered as teas, infusions, tinctures, or encapsulated powders. The appropriate method of administration depends on the specific herb and the individual’s preference and tolerance.
Question 4: Are there potential side effects or interactions with herbal treatments for gastroenteritis?
Yes, herbal remedies can have side effects and may interact with medications. For example, licorice root can elevate blood pressure, and certain herbs can interfere with medication absorption. Consulting a healthcare provider is crucial to assess potential risks.
Question 5: How effective are botanical treatments for gastroenteritis, according to scientific research?
The scientific evidence supporting the efficacy of botanical treatments for gastroenteritis varies. Some herbs, such as ginger for nausea, have demonstrated effectiveness in clinical trials. However, further research is needed to fully evaluate the efficacy and safety of many other herbal remedies.
Question 6: Can botanical treatments prevent the spread of gastroenteritis?
Botanical treatments primarily address the symptoms of gastroenteritis and are not generally considered effective in preventing its spread. Proper hygiene practices, such as frequent handwashing, are essential for preventing the transmission of infectious agents.
The responsible and informed use of botanical remedies in gastroenteritis management necessitates a comprehensive understanding of their potential benefits, risks, and limitations. Medical guidance is paramount.
The subsequent section delves into specific considerations for vulnerable populations and the integration of botanical approaches within a broader management strategy.
Conclusion
The investigation of gastroenteritis herbal treatment reveals a spectrum of potential interventions, ranging from symptom management to microbiome support. The application of these botanicals hinges on a careful consideration of individual patient characteristics, the specific etiology of the condition, and potential interactions with conventional therapies. The integration of traditional knowledge with contemporary scientific inquiry is paramount in discerning effective and safe treatment protocols.
Continued rigorous research, focusing on standardized herbal preparations and well-defined clinical endpoints, is essential to solidify the role of gastroenteritis herbal treatment within evidence-based medical practice. Responsible application necessitates informed decision-making and the prioritization of patient safety.