The employment of botanical remedies to address elevated levels of a specific lipid in the bloodstream represents a growing area of interest within complementary and alternative medicine. This approach involves utilizing plants and their extracts, often in conjunction with dietary and lifestyle modifications, with the goal of modulating lipid profiles.
Interest in non-pharmaceutical interventions for managing health conditions stems from various factors, including a desire for natural options and a proactive approach to wellness. Historically, many cultures have long traditions of using plants for medicinal purposes, informing contemporary practices. The potential benefits may encompass improved well-being, reduced reliance on synthetic drugs, and the potential for fewer adverse effects.
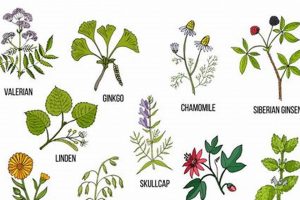
The following sections will explore specific botanical agents studied for their effects on lipid metabolism, examining the evidence supporting their use, and discussing potential considerations regarding safety and efficacy.
Guidance on Botanical Approaches to Lipid Management
The following recommendations are provided for individuals exploring the use of plant-based interventions to assist in maintaining healthy lipid levels. These suggestions should be viewed as complementary to conventional medical advice and not as a replacement for prescribed treatments.
Tip 1: Prioritize Consultation. A thorough discussion with a qualified healthcare provider is essential before initiating any plant-based regimen. This ensures compatibility with existing medications, addresses potential contraindications, and establishes appropriate monitoring strategies.
Tip 2: Embrace Dietary Modifications. Integrating heart-healthy foods rich in soluble fiber, such as oats, beans, and fruits, can synergistically enhance the impact of botanical agents. Limiting saturated and trans fats remains a crucial component of overall lipid management.
Tip 3: Select Standardized Extracts. When choosing a botanical product, opt for standardized extracts from reputable manufacturers. Standardization ensures consistent levels of bioactive compounds, promoting predictable therapeutic effects.
Tip 4: Monitor Lipid Profiles. Regular monitoring of lipid parameters through laboratory testing allows for objective evaluation of the intervention’s effectiveness and facilitates timely adjustments to the treatment plan, if necessary.
Tip 5: Engage in Regular Physical Activity. Consistent aerobic exercise, such as brisk walking or cycling, complements dietary and botanical interventions by promoting overall cardiovascular health and favorably influencing lipid metabolism.
Tip 6: Be Aware of Potential Interactions. Certain plant-derived substances may interact with prescription medications, affecting their efficacy or increasing the risk of adverse events. Diligence in reporting all supplements to a healthcare professional is imperative.
Tip 7: Maintain Realistic Expectations. Botanical interventions typically yield gradual results, requiring sustained adherence and patience. Setting realistic goals and fostering a long-term perspective is conducive to successful outcomes.
Adopting a comprehensive approach that integrates informed decision-making, lifestyle modifications, and appropriate monitoring can optimize the potential benefits of plant-based interventions for supporting healthy lipid levels.
The subsequent sections will delve into considerations regarding the long-term sustainability of botanical approaches to lipid management.
1. Safety Considerations
The safe implementation of botanical interventions for cholesterol management requires meticulous attention to detail, acknowledging that substances of natural origin are not inherently risk-free. Individual responses can vary significantly, and potential adverse effects must be carefully weighed against anticipated benefits. A proactive approach to risk mitigation is paramount.
- Hepatic and Renal Function
Certain botanical compounds may exert stress on the liver and kidneys, potentially exacerbating pre-existing conditions or causing organ damage. Baseline assessment of hepatic and renal function, followed by periodic monitoring, is advisable to detect any signs of compromise. Individuals with a history of liver or kidney disease should proceed with extreme caution.
- Herb-Drug Interactions
Numerous botanical agents possess the capacity to interact with pharmaceutical medications, either enhancing or diminishing their intended effects. For instance, certain herbs may potentiate the anticoagulant effects of warfarin, increasing the risk of bleeding. A comprehensive review of all medications, including over-the-counter drugs and other supplements, is crucial to identify and mitigate potential interactions.
- Allergic Reactions and Sensitivities
Individuals may exhibit allergic reactions or sensitivities to specific botanical compounds, manifesting as skin rashes, gastrointestinal distress, or, in rare cases, anaphylaxis. A thorough allergy history should be obtained prior to initiating any herbal regimen. Starting with low doses and gradually increasing the dosage allows for monitoring of potential adverse reactions.
- Quality Control and Adulteration
The botanical supplement industry is subject to varying levels of quality control, raising concerns about product adulteration with contaminants or inaccurate labeling. Selecting products from reputable manufacturers that adhere to Good Manufacturing Practices (GMP) is essential to minimize the risk of exposure to harmful substances. Third-party testing for purity and potency can provide an additional layer of assurance.
The multifaceted nature of safety considerations underscores the necessity of a collaborative approach involving healthcare providers, pharmacists, and informed patients. A diligent assessment of potential risks, coupled with proactive monitoring and adherence to quality control standards, is crucial to optimize the safety profile of botanical interventions employed in cholesterol management. The following sections will address considerations related to the clinical efficacy of various botanical agents.
2. Clinical Efficacy
The connection between clinical efficacy and interventions targeting elevated lipid levels through botanical means is paramount. Clinical efficacy, defined as the demonstrated ability of an intervention to produce a beneficial effect under controlled experimental conditions, serves as the cornerstone for evaluating the merit of any treatment modality. In the context of botanical treatments for high cholesterol, the absence of robust clinical evidence renders the intervention speculative and potentially unreliable. Without rigorous clinical trials, the observed effects may be attributable to confounding variables, placebo effects, or publication bias, rather than the inherent properties of the botanical agent itself.
Establishing clinical efficacy requires adherence to the scientific method, encompassing well-designed randomized controlled trials (RCTs) with appropriate sample sizes, clear inclusion and exclusion criteria, standardized treatment protocols, objective outcome measures, and rigorous statistical analysis. Positive results from well-executed clinical trials provide evidence that the botanical intervention is capable of lowering lipid levels to a clinically significant extent. Conversely, negative or inconclusive results cast doubt on the intervention’s value and necessitate further investigation or the consideration of alternative approaches. For example, while some studies suggest a modest effect of red yeast rice on lowering LDL cholesterol, concerns remain regarding the consistency of active compound concentrations and potential contamination, warranting cautious interpretation and further research. The use of plant sterols, in contrast, is supported by stronger evidence, with numerous clinical trials demonstrating their ability to reduce LDL cholesterol by interfering with intestinal cholesterol absorption.
In summary, clinical efficacy is an indispensable component of responsible and evidence-based botanical approaches to cholesterol management. A thorough understanding of the existing clinical evidence, its limitations, and the need for ongoing research is essential for healthcare professionals and individuals considering these interventions. The presence of robust clinical efficacy data instills confidence in the intervention’s potential to yield tangible benefits, whereas its absence underscores the need for caution and a critical appraisal of alternative strategies. The subsequent discussion will address the importance of product standardization in ensuring the reliability and consistency of botanical interventions.
3. Product Standardization
Product standardization is a critical aspect of herbal interventions aimed at managing cholesterol levels. This process involves ensuring that each dose of a botanical product contains a consistent and quantifiable amount of the active compound(s) responsible for its therapeutic effect. The inherent variability in plant material, influenced by factors such as growing conditions, harvesting methods, and processing techniques, necessitates standardization to mitigate inconsistent outcomes and ensure predictable clinical effects. Without standardization, the concentration of active constituents may fluctuate significantly between batches, leading to unpredictable and potentially ineffective treatments. For instance, a product labeled as containing a specific herb known to lower cholesterol might, in reality, contain a significantly lower quantity of the active compounds, rendering it ineffective.
The absence of product standardization can have serious implications for the efficacy and safety of herbal treatments. Patients may experience inconsistent or non-existent therapeutic benefits, leading to frustration and potentially deterring them from pursuing appropriate medical care. Furthermore, inconsistent potency increases the risk of adverse effects, as dosages become difficult to control. Consider the example of milk thistle, often used for liver support. Different preparations of milk thistle can vary widely in their silymarin content, the active compound responsible for its effects. Standardization ensures that patients receive a consistent dose of silymarin, maximizing its potential benefits while minimizing the risk of unexpected side effects. Therefore, when considering herbal treatments for cholesterol management, it is crucial to seek out products that have undergone rigorous standardization processes, often indicated on the label or through third-party certifications.
In conclusion, product standardization is not merely a quality control measure, but a fundamental prerequisite for ensuring the efficacy and safety of botanical interventions intended to address elevated cholesterol levels. Consistent dosages of active compounds enhance therapeutic predictability, minimize the risk of adverse events, and instill confidence in the reliability of herbal treatments. The absence of standardization undermines the potential benefits of herbal therapies and poses a significant challenge to their integration into evidence-based healthcare practices.
4. Potential Interactions
The risk of pharmacological interactions is a significant concern when considering botanical interventions for managing cholesterol levels. Combining herbal remedies with conventional medications can lead to unpredictable outcomes, potentially compromising treatment efficacy or increasing the risk of adverse events. A thorough understanding of these potential interactions is crucial for ensuring patient safety and optimizing therapeutic outcomes.
- Cytochrome P450 Enzyme Modulation
Many botanical compounds can either inhibit or induce cytochrome P450 (CYP) enzymes, a family of enzymes responsible for metabolizing a large percentage of drugs. For example, St. John’s Wort, an herbal antidepressant, is a known CYP3A4 inducer, which can accelerate the metabolism of statins, thereby reducing their effectiveness in lowering cholesterol. Conversely, other herbs may inhibit CYP enzymes, increasing statin levels and the risk of myopathy. Understanding these enzymatic interactions is crucial for avoiding unwanted drug level alterations.
- Pharmacodynamic Interactions
Pharmacodynamic interactions occur when two or more substances have additive, synergistic, or antagonistic effects on the body. Garlic, for instance, has mild antiplatelet properties. When combined with anticoagulant medications like warfarin or antiplatelet drugs like aspirin, the risk of bleeding may be significantly increased. Such pharmacodynamic interactions can lead to serious adverse events if not carefully monitored and managed.
- Absorption and Bioavailability Alterations
Certain herbs can affect the absorption and bioavailability of cholesterol-lowering medications. For example, the consumption of high-fiber herbs or supplements alongside statins may reduce the absorption of the statin from the gastrointestinal tract, decreasing its effectiveness. Separating the administration of these substances by several hours may mitigate this interaction; however, awareness of this potential effect is essential for ensuring optimal drug absorption.
- Competition for Transport Proteins
Some botanical compounds and medications may compete for the same transport proteins in the body, affecting their distribution and elimination. This competition can alter the concentration of both substances in the bloodstream, potentially leading to toxicity or reduced efficacy. Further research is needed to fully elucidate the transport protein interactions of common herbal remedies used for cholesterol management.
The complexity of potential interactions underscores the importance of a comprehensive medication review by a qualified healthcare professional before initiating any herbal treatment for cholesterol. Transparency regarding all supplements and medications is essential for identifying and mitigating potential risks. Careful monitoring and, when necessary, dose adjustments can help ensure the safe and effective use of both conventional and botanical approaches to cholesterol management.
5. Lipid Monitoring
Regular assessment of lipid profiles through laboratory testing is an indispensable component of any cholesterol management strategy, including those incorporating botanical interventions. Consistent monitoring provides objective data on the effectiveness of the chosen approach and allows for timely adjustments to optimize therapeutic outcomes. Without diligent monitoring, individuals risk unknowingly persisting with ineffective treatments or experiencing adverse effects that could have been mitigated with early detection.
- Baseline Assessment and Trend Tracking
A comprehensive lipid panel, encompassing total cholesterol, LDL-cholesterol, HDL-cholesterol, and triglycerides, should be obtained prior to initiating any herbal treatment. This baseline assessment establishes a reference point against which subsequent changes can be compared. Regular follow-up testing, typically at intervals of 3-6 months, enables the tracking of trends and identification of patterns in lipid parameters, providing valuable insights into the intervention’s impact.
- Efficacy Evaluation and Dose Adjustment
Serial lipid measurements provide the empirical data necessary to evaluate the efficacy of a given herbal treatment. If lipid parameters fail to improve adequately after a reasonable period, adjustments to the dosage, the addition of complementary interventions, or a re-evaluation of the treatment plan may be warranted. Objective data from lipid monitoring informs these decisions, preventing reliance on subjective perceptions or anecdotal evidence.
- Safety Monitoring and Adverse Effect Detection
Lipid monitoring can also serve as a valuable tool for detecting potential adverse effects of herbal treatments. For example, some botanical agents may, in rare cases, elevate liver enzymes or cause changes in other biochemical markers. Periodic monitoring of liver function and other relevant parameters can facilitate the early identification of such adverse effects, allowing for prompt intervention to mitigate potential harm.
- Personalized Treatment Optimization
Individual responses to herbal treatments can vary significantly, influenced by factors such as genetics, lifestyle, and underlying health conditions. Lipid monitoring enables the personalization of treatment strategies based on individual responses. By closely tracking lipid parameters, healthcare providers can tailor the treatment plan to optimize its effectiveness and minimize potential adverse effects for each patient.
In summary, lipid monitoring is not merely an ancillary procedure but an essential element of any cholesterol management protocol that incorporates botanical interventions. It provides the objective data necessary to evaluate efficacy, monitor safety, guide treatment adjustments, and personalize care. A proactive approach to lipid monitoring empowers individuals and healthcare providers to make informed decisions, ultimately enhancing the effectiveness and safety of herbal treatments for cholesterol management.
6. Lifestyle Integration
The efficacy of botanical interventions for managing cholesterol levels is significantly enhanced when combined with holistic lifestyle modifications. This integrated approach acknowledges that lipid profiles are influenced by multiple factors, extending beyond pharmacological or herbal interventions alone. Lifestyle integration encompasses dietary adjustments, regular physical activity, stress management techniques, and smoking cessation, all of which can synergistically complement the effects of herbal remedies. The absence of such integration may limit the potential benefits of botanical treatments, potentially resulting in suboptimal outcomes.
Dietary modifications, in particular, play a crucial role in optimizing the impact of herbal remedies. A diet rich in saturated and trans fats can undermine the cholesterol-lowering effects of even the most potent botanical agents. Conversely, a diet abundant in soluble fiber, fruits, vegetables, and lean protein promotes healthy lipid metabolism, creating a more favorable environment for herbal interventions to exert their effects. For example, an individual consuming a diet high in processed foods and saturated fats while simultaneously taking a botanical supplement marketed for cholesterol reduction is unlikely to experience significant benefits. In contrast, an individual adhering to a heart-healthy diet and incorporating regular exercise, alongside a carefully selected herbal remedy, is more likely to achieve meaningful improvements in their lipid profile. Similarly, regular physical activity can improve HDL cholesterol levels, reduce blood pressure, and enhance insulin sensitivity, further complementing the effects of botanical treatments. Stress management techniques, such as meditation or yoga, can also indirectly influence lipid levels by reducing the release of cortisol, a hormone that can contribute to elevated cholesterol. Smoking cessation is another essential component of lifestyle integration, as smoking negatively impacts lipid profiles and increases the risk of cardiovascular disease.
Lifestyle integration represents a multifaceted approach to cholesterol management, recognizing that botanical treatments are most effective when incorporated into a broader framework of healthy habits. By addressing the underlying lifestyle factors that contribute to elevated cholesterol, individuals can maximize the potential benefits of herbal remedies and achieve more sustainable improvements in their cardiovascular health. The synergistic effects of lifestyle modifications and botanical interventions underscore the importance of a holistic perspective in addressing complex health challenges.
Frequently Asked Questions Regarding Botanical Approaches to Cholesterol Management
The following section addresses common inquiries pertaining to the use of botanical agents as a component of cholesterol management. The information presented is intended to provide clarification and guidance, and should not be interpreted as medical advice.
Question 1: What constitutes a scientifically substantiated herbal treatment for cholesterol?
A scientifically substantiated approach necessitates evidence from rigorous clinical trials, demonstrating a statistically significant and clinically relevant reduction in LDL-cholesterol or other relevant lipid parameters. The botanical agent should be well-characterized, and the product should adhere to stringent quality control standards.
Question 2: Are botanical interventions a suitable substitute for statin medications?
The decision to utilize botanical interventions in lieu of statin medications should be made in consultation with a qualified healthcare provider. In some cases, botanical agents may be appropriate for individuals with mild hypercholesterolemia or those unable to tolerate statins. However, for individuals at high cardiovascular risk, statins remain the primary therapeutic modality.
Question 3: What are the potential risks associated with combining herbal treatments with conventional cholesterol-lowering medications?
The concomitant use of botanical agents and conventional medications can lead to unpredictable interactions, potentially affecting the efficacy or safety of either treatment. Certain herbs may alter the metabolism or absorption of statins, requiring careful monitoring and dose adjustments. Open communication with a healthcare provider is crucial to mitigate these risks.
Question 4: How does product standardization impact the effectiveness of herbal treatments for cholesterol?
Product standardization ensures that each dose of a botanical product contains a consistent and quantifiable amount of the active compound(s) responsible for its therapeutic effect. This uniformity is essential for achieving predictable clinical outcomes and minimizing variability in response. Non-standardized products may contain inconsistent levels of active constituents, rendering them less effective or potentially unsafe.
Question 5: How quickly can improvements in cholesterol levels be expected with herbal treatments?
The timeline for observing improvements in cholesterol levels with botanical interventions varies depending on the individual, the specific agent used, and the concomitant lifestyle modifications implemented. Some individuals may experience noticeable changes within several weeks, while others may require several months. Consistent adherence to the treatment plan and regular lipid monitoring are essential for tracking progress.
Question 6: Where can one find reliable information regarding the safety and efficacy of specific herbal treatments for cholesterol?
Reliable information can be obtained from peer-reviewed scientific publications, reputable medical websites, and consultations with qualified healthcare professionals, including physicians, pharmacists, and registered dietitians. It is important to critically evaluate information from unverified sources and to prioritize evidence-based recommendations.
The responsible and informed utilization of botanical agents for cholesterol management necessitates a thorough understanding of the available evidence, potential risks, and the importance of lifestyle integration.
The subsequent section will provide guidance on identifying reputable sources of botanical products.
Conclusion
This exploration of herbal treatment for cholesterol has underscored the complexities and nuances associated with employing botanical agents for lipid management. Key points include the necessity of clinical evidence, the importance of product standardization, the potential for herb-drug interactions, and the critical role of lifestyle integration. These factors collectively influence the safety and efficacy of botanical interventions.
Responsible utilization of herbal treatment for cholesterol necessitates a cautious and informed approach. Prioritizing consultation with qualified healthcare professionals and adhering to evidence-based principles is essential for maximizing potential benefits while minimizing risks. Further research is needed to fully elucidate the efficacy and safety profiles of specific botanical agents, ultimately informing evidence-based guidelines for their use.