Substances derived from plants, typically ingested orally, are sometimes employed with the intention of supporting the function of a specific organ involved in metabolic processes. These natural preparations are often complex mixtures of bioactive compounds believed to promote detoxification and overall well-being. Historically, such botanical remedies have been utilized in various cultures for purported therapeutic effects on the body’s primary filtration system.
The perceived advantages of these plant-based supplements stem from the belief that they can enhance the organ’s natural ability to process toxins, potentially improving digestion, increasing energy levels, and contributing to overall vitality. Traditional medicine systems have long emphasized the importance of maintaining a healthy filtration system, citing its critical role in supporting the body’s natural equilibrium. The historical use of these substances can be traced back centuries, with documented applications in traditional healing practices across different geographic regions.
The subsequent discussion will delve into the specific components often found in these formulations, examining the available scientific evidence regarding their efficacy and potential risks, and exploring alternative approaches to maintaining the health of this essential metabolic organ.
Guidance Regarding Botanical Liver Support
The following points offer considerations regarding the use of plant-derived compounds aimed at supporting the liver’s function. It is imperative to consult with a qualified healthcare professional before initiating any new regimen, especially if pre-existing medical conditions are present or pharmaceutical medications are being taken.
Tip 1: Research Specific Ingredients: Before consumption, rigorously examine the active constituents within any herbal product. Scrutinize scientific literature regarding the efficacy and potential adverse effects associated with ingredients such as milk thistle, dandelion root, or artichoke extract.
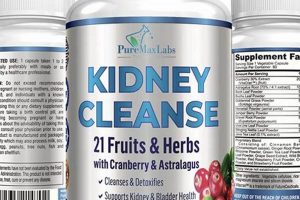
Tip 2: Verify Product Quality: Prioritize products sourced from reputable manufacturers who adhere to stringent quality control standards. Look for certifications indicating third-party testing for purity and potency. Avoid products with ambiguous labeling or unsupported claims.
Tip 3: Understand Dosage Guidelines: Adhere precisely to recommended dosage instructions provided by the manufacturer or a qualified healthcare provider. Exceeding the recommended dosage may increase the risk of adverse reactions without necessarily enhancing the intended benefit.
Tip 4: Monitor for Adverse Effects: Vigilantly observe for any signs of adverse reactions following initiation of a botanical regimen. Common side effects may include gastrointestinal upset, skin rash, or allergic reactions. Discontinue use and seek medical attention if concerning symptoms arise.
Tip 5: Consider Interactions with Medications: Be aware of potential interactions between botanical compounds and prescription or over-the-counter medications. Certain herbs can alter the metabolism of drugs, leading to reduced efficacy or increased toxicity. Consult with a pharmacist or physician to assess potential interactions.
Tip 6: Emphasize a Holistic Approach: Recognize that botanical remedies are not a substitute for a healthy lifestyle. Prioritize a balanced diet, regular physical activity, adequate hydration, and avoidance of excessive alcohol consumption and tobacco use.
Tip 7: Acknowledge Limitations of Evidence: Exercise caution regarding exaggerated claims of efficacy. While some botanical compounds may offer potential benefits, the scientific evidence supporting their use for promoting liver health is often limited or inconclusive. Critically evaluate available information and consult with a healthcare professional for personalized advice.
Adherence to these guidelines can assist in making informed decisions regarding the use of plant-derived substances intended to support liver function.
The subsequent section will explore alternative strategies for maintaining liver health, independent of botanical supplementation.
1. Botanical Composition
The botanical composition of preparations marketed for hepatic support directly influences their potential efficacy and safety. A thorough understanding of the constituents, their concentrations, and their interactions is paramount for informed decision-making.
- Active Compounds and Mechanisms of Action
The presence and concentration of specific bioactive molecules determine the purported effects. For example, silymarin, a complex of flavonolignans found in milk thistle (Silybum marianum), is often cited for its antioxidant and anti-inflammatory properties, potentially mitigating hepatic injury. However, the precise mechanisms of action of silymarin and other botanical compounds remain subjects of ongoing research.
- Variability and Standardization
The chemical composition of plant materials can vary significantly due to factors such as growing conditions, harvesting practices, and processing methods. This variability can lead to inconsistencies in the potency and efficacy of herbal products. Standardization aims to ensure consistent levels of specific marker compounds, but standardization practices may differ among manufacturers, and the relevance of specific marker compounds to overall efficacy is not always fully established.
- Potential for Synergistic or Antagonistic Effects
Herbal preparations typically contain a multitude of compounds, and interactions between these compounds can influence their overall effects. Synergistic effects may enhance the therapeutic benefits, while antagonistic effects may diminish or negate them. The complexity of these interactions makes it challenging to predict the overall effect of a complex botanical mixture based solely on the known properties of individual constituents.
- Presence of Contaminants and Adulterants
The botanical composition may be compromised by the presence of contaminants, such as heavy metals, pesticides, or microbial pathogens. Adulteration, the deliberate or unintentional substitution of one plant material for another, also poses a risk. These factors can compromise the safety and efficacy of herbal products and underscore the importance of sourcing from reputable manufacturers who adhere to stringent quality control standards.
In essence, the detailed botanical composition of “liver cleansing herbal” supplements is not merely a list of ingredients but a complex interplay of factors influencing both intended benefits and potential harms. Rigorous analysis of the active compounds, understanding variability, potential synergistic effects, and control of contaminants are all necessary to ensure the efficacy and safety of such preparations. The absence of thorough quality control can introduce significant risks, emphasizing the need for consumers and practitioners to critically evaluate the botanical composition and source of herbal liver support products.
2. Quality Verification
Quality verification constitutes an indispensable element in the context of plant-derived preparations intended to support hepatic function. The inherent variability in botanical materials, encompassing factors such as growing conditions, harvesting methods, and processing techniques, introduces a significant potential for inconsistencies in the composition and potency of these products. Consequently, rigorous quality verification procedures are essential to ensure product integrity and mitigate the risks associated with substandard or adulterated formulations. Without stringent quality controls, the promised beneficial effects of botanical liver support may be compromised, or, more seriously, products may pose a direct threat to consumer health. For instance, preparations contaminated with heavy metals, pesticides, or microorganisms could exacerbate existing liver conditions or cause new forms of hepatic damage. Similarly, the substitution of authentic herbal ingredients with inferior or even harmful substitutes represents a tangible danger in the absence of thorough quality verification protocols.
The practical significance of quality verification extends beyond mere safety concerns. Accurate identification and quantification of active compounds are critical for establishing appropriate dosage recommendations and predicting potential therapeutic effects. If the concentration of key bioactive molecules, such as silymarin in milk thistle extracts, deviates substantially from the label claim, the intended clinical benefits may not materialize, or unintended adverse reactions may occur. Furthermore, the assessment of product stability over time is an important aspect of quality verification. Degradation of active compounds during storage or transit can lead to a reduction in efficacy, rendering the product ineffective even if it initially met quality standards. Real-world examples of herbal product contamination and adulteration underscore the necessity of robust quality verification programs that encompass both raw material analysis and finished product testing. Independent third-party certification, such as those offered by organizations like the U.S. Pharmacopeia (USP) or NSF International, can provide an additional layer of assurance to consumers.
In conclusion, quality verification is not merely a procedural step but a fundamental safeguard that ensures the safety, efficacy, and consistency of plant-derived liver support products. The absence of rigorous quality control measures can undermine the potential therapeutic benefits and expose consumers to unacceptable health risks. Challenges persist in the implementation of standardized quality verification practices across the herbal industry, but a commitment to transparency, traceability, and independent testing is essential for fostering consumer confidence and promoting the responsible use of botanical medicines.
3. Dosage Regulation
Dosage regulation is a critical determinant of both the safety and efficacy of any intervention, including the consumption of plant-derived substances intended to support liver function. In the realm of these preparations, precise dosage control is not merely a matter of convenience but a fundamental requirement for minimizing potential harm and maximizing any purported therapeutic benefits. The complex chemical composition of botanical materials, combined with individual variations in metabolism and sensitivity, necessitates a cautious and informed approach to dosage regulation.
- Variability in Bioactive Compound Concentration
Plant-derived substances inherently exhibit variability in the concentration of active constituents. Factors such as growing conditions, harvesting techniques, and processing methods can significantly impact the levels of key bioactive compounds. Consequently, even seemingly identical doses of a particular preparation may result in widely differing exposure levels. For example, the silymarin content in milk thistle extracts can vary considerably across different brands and batches. This necessitates a careful evaluation of product standardization and reliable sourcing to ensure consistent dosage.
- Individual Metabolic Differences
Individual variations in hepatic enzyme activity, genetic polymorphisms, and pre-existing medical conditions can significantly influence the metabolism and clearance of botanical compounds. What constitutes a safe and effective dose for one individual may be ineffective or even toxic for another. Patients with impaired liver function, for instance, may exhibit reduced ability to metabolize certain compounds, leading to increased systemic exposure and a higher risk of adverse effects. Therefore, dosage adjustments may be necessary based on individual health status and potential drug interactions.
- Potential for Drug Interactions
Plant-derived substances can interact with prescription and over-the-counter medications, potentially altering their pharmacokinetic or pharmacodynamic properties. Certain botanical compounds may inhibit or induce hepatic enzymes involved in drug metabolism, leading to increased or decreased drug levels in the body. For example, St. John’s Wort, although not typically associated with liver support, is a well-known inducer of CYP3A4, a major hepatic enzyme involved in the metabolism of numerous drugs. It is therefore crucial to consider potential drug interactions when determining the appropriate dosage of any herbal preparation.
- Dose-Response Relationship and Toxicity Thresholds
The relationship between dosage and therapeutic effect may not be linear, and there is often a threshold beyond which increasing the dose does not result in proportionally greater benefits and may, in fact, increase the risk of adverse effects. Some botanical compounds exhibit a narrow therapeutic window, meaning that the difference between a safe and effective dose and a toxic dose is relatively small. Careful titration and monitoring are therefore essential to identify the optimal dosage and minimize the risk of toxicity. For example, certain pyrrolizidine alkaloids, found in some herbal remedies, can cause hepatic veno-occlusive disease if ingested in sufficient quantities.
In summary, dosage regulation is a multifaceted and essential consideration in the context of plant-derived liver support preparations. Variability in bioactive compound concentration, individual metabolic differences, potential for drug interactions, and the dose-response relationship all contribute to the complexity of determining appropriate dosage regimens. A cautious and informed approach, guided by scientific evidence and consultation with healthcare professionals, is paramount to ensure the safe and effective use of these substances. An understanding of these challenges strengthens the perspective related to proper dosage practices.
4. Potential Interactions
Potential interactions represent a significant concern when considering the use of plant-derived substances marketed for hepatic support. The concurrent consumption of these preparations with prescription medications, over-the-counter drugs, or even other herbal remedies can lead to unpredictable and potentially harmful outcomes. These interactions arise from the complex interplay of biochemical processes that govern drug metabolism, transport, and receptor binding.
- Cytochrome P450 Modulation
Many herbal constituents can modulate the activity of cytochrome P450 (CYP) enzymes, a family of hepatic enzymes responsible for metabolizing a substantial proportion of pharmaceutical drugs. Some herbs may induce CYP enzyme activity, leading to accelerated drug metabolism and reduced drug efficacy. Conversely, other herbs may inhibit CYP enzymes, resulting in decreased drug metabolism and increased drug concentrations, potentially leading to toxicity. For instance, St. John’s Wort, a potent CYP3A4 inducer, can reduce the effectiveness of medications such as cyclosporine, warfarin, and oral contraceptives. Although St. John’s Wort is not primarily used for liver support, the principle applies to other herbal substances with CYP-modulating properties.
- Transport Protein Inhibition
Certain herbal compounds can inhibit transport proteins, such as P-glycoprotein (P-gp), which play a critical role in the absorption, distribution, and elimination of drugs. Inhibition of P-gp can lead to increased drug concentrations in certain tissues and decreased drug concentrations in others, potentially altering the drug’s therapeutic effect and increasing the risk of adverse events. For example, some flavonoids found in herbal extracts have been shown to inhibit P-gp activity, affecting the bioavailability of drugs such as digoxin and certain chemotherapeutic agents.
- Additive or Synergistic Effects
The concurrent use of multiple substances with similar pharmacological properties can result in additive or synergistic effects, potentially leading to exaggerated or unexpected outcomes. For instance, combining a plant-derived substance with known anticoagulant properties, such as high-dose garlic or ginger, with warfarin or other anticoagulant drugs can increase the risk of bleeding complications. Similarly, combining multiple herbs with sedative or hypotensive effects can potentiate these effects, increasing the risk of falls or excessive drowsiness.
- Competition for Binding Sites
Some herbal compounds may compete with drugs for binding sites on plasma proteins or cellular receptors, potentially altering the distribution and activity of the drug. This competition can lead to decreased drug efficacy or increased drug toxicity, depending on the specific drug and herbal substance involved. For example, certain herbal constituents with high affinity for albumin, a major plasma protein, can displace drugs that are also highly bound to albumin, increasing the free concentration of the drug in the plasma and potentially leading to increased toxicity.
The potential for interactions between plant-derived liver support preparations and conventional medications is a complex and often underappreciated consideration. These interactions can significantly alter the pharmacokinetic and pharmacodynamic properties of drugs, leading to unpredictable and potentially harmful outcomes. A thorough understanding of the potential mechanisms of interaction, coupled with careful monitoring and consultation with healthcare professionals, is essential to minimize the risks associated with concurrent use of these substances. Caution is warranted to avoid possible complications.
5. Adverse Reactions
Consumption of plant-derived substances intended for hepatic support, while often perceived as natural and benign, is not without the potential for adverse reactions. These reactions can range from mild gastrointestinal disturbances to severe hepatic injury, necessitating a careful evaluation of potential risks before initiating any such regimen. The complex chemical composition of these preparations, coupled with individual variations in metabolism and susceptibility, contributes to the diversity and unpredictability of adverse events.
Adverse reactions can stem from several factors, including direct hepatotoxicity of certain herbal constituents, allergic reactions to specific plant components, and interactions with conventional medications. For example, pyrrolizidine alkaloids (PAs), found in some herbal remedies, are known hepatotoxins and can cause hepatic veno-occlusive disease, a severe and potentially fatal condition. Allergic reactions, though less common, can manifest as skin rashes, angioedema, or even anaphylaxis. Furthermore, the potential for drug interactions can exacerbate existing medical conditions or lead to unforeseen adverse events. The severity of adverse reactions is often dose-dependent, with higher doses generally associated with a greater risk of harm. However, even low doses can trigger adverse reactions in susceptible individuals.
Understanding the potential for adverse reactions is crucial for informed decision-making regarding the use of plant-derived substances for liver support. Individuals with pre-existing liver disease, impaired kidney function, or a history of allergic reactions should exercise particular caution. Thorough product evaluation, adherence to recommended dosage guidelines, and vigilant monitoring for any signs of adverse events are essential. Healthcare professionals should be consulted to assess individual risk factors and provide guidance on the safe and appropriate use of these preparations. While plant-derived substances may offer potential benefits for hepatic health, it is imperative to acknowledge and mitigate the inherent risks associated with their consumption.
6. Holistic Integration
Holistic integration, within the context of liver support, emphasizes a comprehensive approach that extends beyond solely relying on plant-derived substances. This perspective acknowledges that the liver’s health is intricately connected to overall well-being, encompassing dietary habits, lifestyle factors, and mental-emotional balance. Therefore, while botanical remedies may play a supportive role, they are most effective when integrated into a broader strategy aimed at promoting optimal liver function and overall health.
- Dietary Modifications
A diet rich in whole, unprocessed foods, including fruits, vegetables, and lean proteins, supports liver function by providing essential nutrients and antioxidants while minimizing the intake of processed foods, saturated fats, and excessive sugar, which can contribute to hepatic stress. For instance, incorporating foods known to support liver detoxification pathways, such as cruciferous vegetables (broccoli, cauliflower, Brussels sprouts), can enhance the liver’s ability to process and eliminate toxins. A holistic approach considers these dietary factors as foundational, complementing any use of plant-derived liver support preparations.
- Lifestyle Adjustments
Regular physical activity, adequate sleep, and stress management techniques are crucial components of a holistic approach to liver health. Exercise enhances circulation, promotes detoxification through sweat, and helps maintain a healthy weight, reducing the risk of non-alcoholic fatty liver disease (NAFLD). Sufficient sleep allows the liver to repair and regenerate, while stress management techniques, such as meditation or yoga, can mitigate the negative impact of chronic stress on liver function. These lifestyle modifications work synergistically with plant-derived substances to optimize liver health.
- Minimizing Toxin Exposure
Reducing exposure to environmental toxins, such as pollutants, pesticides, and heavy metals, is an essential aspect of holistic liver support. This may involve choosing organic foods, using natural cleaning products, and avoiding exposure to industrial chemicals. The liver is the primary organ responsible for detoxifying the body, and minimizing the burden of environmental toxins allows it to function more efficiently and effectively. In conjunction with plant-derived remedies, a focus on toxin reduction promotes a healthier internal environment.
- Addressing Underlying Conditions
Underlying medical conditions, such as diabetes, obesity, and autoimmune disorders, can significantly impact liver health. A holistic approach emphasizes addressing these underlying conditions through appropriate medical care and lifestyle modifications. Managing blood sugar levels, maintaining a healthy weight, and addressing autoimmune inflammation are all crucial steps in protecting the liver from further damage. Plant-derived substances may offer supportive benefits, but they are not a substitute for addressing underlying medical conditions.
In conclusion, holistic integration recognizes that liver health is interconnected with overall well-being and emphasizes a comprehensive approach that encompasses dietary modifications, lifestyle adjustments, toxin reduction, and addressing underlying conditions. While plant-derived substances may play a supportive role, they are most effective when integrated into this broader context. By adopting a holistic perspective, individuals can optimize liver function, promote overall health, and minimize the risk of adverse events associated with the use of plant-derived remedies. An approach to liver health should include an awareness that holistic is interconnected.
7. Evidence Limitations
The domain of plant-derived substances marketed for hepatic support is characterized by significant evidentiary constraints. Rigorous scientific substantiation supporting the efficacy and safety of many of these formulations is often lacking. This paucity of robust evidence stems from several factors, including methodological challenges in conducting clinical trials on complex herbal mixtures, publication bias favoring positive results, and a lack of standardized manufacturing practices. Consequently, the marketing claims associated with many preparations may not be fully supported by the available data. An example is the variability in the chemical composition of milk thistle extracts, a commonly used ingredient in liver support supplements. While some studies suggest potential benefits of silymarin, the active compound in milk thistle, other studies have yielded inconsistent or negative results. The lack of standardization in silymarin content across different products further complicates the interpretation of these findings.
The implications of these evidentiary limitations are considerable. Consumers may be misled into believing that these products offer guaranteed benefits, despite the absence of conclusive scientific proof. Furthermore, the use of unproven remedies may delay or replace conventional medical treatment for liver diseases, potentially leading to adverse health outcomes. Clinicians face challenges in providing evidence-based recommendations to patients regarding the use of plant-derived liver support. The limited availability of high-quality clinical trial data makes it difficult to assess the true benefits and risks of these interventions, hindering informed decision-making. This necessitates a cautious and critical approach to evaluating the available evidence, recognizing the inherent limitations of observational studies and preclinical data. It is vital to maintain awareness and seek out the best information available to make sensible decisions about liver health and supplementation.
In summary, the use of plant-derived substances for hepatic support is often predicated on limited and inconclusive evidence. Methodological challenges, publication bias, and a lack of standardization contribute to this evidentiary gap. A critical assessment of marketing claims, coupled with a reliance on evidence-based medical guidance, is essential to protect consumers and ensure that these substances are used safely and appropriately. The field requires increased investment in rigorous clinical research to clarify the true potential and limitations of plant-derived liver support preparations, thereby improving the quality of care for individuals with liver diseases. It is equally important to continue developing the body of research surrounding the effects of specific “liver cleansing herbal” ingredients to foster awareness and informed decisions.
Frequently Asked Questions Regarding Botanical Liver Support
The following addresses commonly raised inquiries pertaining to the use of plant-derived substances intended to support hepatic function. The information presented is intended to provide a balanced and informative perspective, emphasizing the importance of evidence-based decision-making.
Question 1: Are “liver cleansing herbal” products scientifically proven to detoxify the liver?
The term “detoxification” is often used loosely in marketing materials. While the liver plays a crucial role in eliminating toxins, rigorous scientific evidence supporting the ability of herbal products to enhance this process beyond the liver’s natural capacity is generally lacking. Some substances may support certain liver functions, but the concept of a “detox” product lacks specific, scientifically validated endpoints.
Question 2: Can “liver cleansing herbal” supplements repair damaged liver tissue?
Some botanical compounds exhibit antioxidant and anti-inflammatory properties, which may theoretically contribute to liver tissue protection. However, conclusive evidence demonstrating the ability of these substances to definitively repair damaged liver tissue is limited. Treatment of liver damage typically requires addressing the underlying cause of the injury, such as alcohol abuse, viral infection, or autoimmune disease.
Question 3: Are all “liver cleansing herbal” ingredients safe for consumption?
Not all herbal ingredients are inherently safe. Some plant-derived substances contain compounds that can be hepatotoxic, meaning they can cause liver damage. Furthermore, potential drug interactions and individual sensitivities must be carefully considered. Consultation with a healthcare professional is advised before initiating any herbal regimen.
Question 4: How can one determine the quality and purity of “liver cleansing herbal” products?
Quality verification is crucial. Look for products manufactured by reputable companies that adhere to Good Manufacturing Practices (GMP). Third-party certifications, such as those from USP or NSF International, can provide an additional level of assurance. Scrutinize product labels for detailed ingredient information and avoid products with ambiguous or unsupported claims.
Question 5: Can “liver cleansing herbal” products prevent liver disease?
There is no conclusive evidence demonstrating that plant-derived substances can definitively prevent liver disease. While a healthy lifestyle, including a balanced diet, regular exercise, and avoidance of excessive alcohol consumption, is crucial for liver health, botanical supplements should not be considered a substitute for these fundamental preventative measures.
Question 6: Are there any potential side effects associated with “liver cleansing herbal” supplements?
Yes, potential side effects can occur. These may include gastrointestinal upset, allergic reactions, and interactions with prescription medications. It is essential to carefully monitor for any signs of adverse reactions and to discontinue use if concerning symptoms arise. Individuals with pre-existing medical conditions should consult with a healthcare professional before using these products.
In essence, the effectiveness and safety of plant-derived substances for hepatic support are subjects of ongoing scientific investigation. Consumers should exercise caution and rely on evidence-based information when making decisions about these products. Consultation with healthcare providers is crucial to minimize the risks associated with herbal interventions.
The following section will explore alternative methods for liver care, including lifestyle adaptations and professional medical assistance.
Conclusion
This exploration of “liver cleansing herbal” underscores the complexities inherent in utilizing plant-derived substances for hepatic support. The analysis has highlighted the critical importance of understanding botanical composition, verifying product quality, regulating dosage, considering potential interactions, recognizing adverse reactions, integrating holistic approaches, and acknowledging the limitations of existing evidence. These elements collectively form a framework for responsible evaluation and informed decision-making regarding these preparations.
Given the nuanced and sometimes uncertain nature of the available evidence, a cautious and critical approach is warranted. Individuals considering the use of “liver cleansing herbal” should prioritize consultation with qualified healthcare professionals to assess individual risk factors, evaluate potential benefits, and ensure that any such regimen is integrated into a comprehensive strategy for liver health. Further rigorous scientific investigation is essential to definitively establish the efficacy and safety of these substances and to provide evidence-based guidance for their appropriate use in clinical practice.