Certain plant-based infusions, while generally considered healthful, present potential risks during gestation. These risks stem from bioactive compounds within the herbs that may impact hormonal balance, uterine contractions, or fetal development. Examples include teas containing ingredients such as pennyroyal, blue cohosh, and black cohosh.
Awareness of potentially harmful herbal constituents is crucial for maternal and fetal well-being. Historically, traditional medicine systems have utilized herbs for various purposes, including pregnancy support; however, not all traditional remedies are safe for contemporary use due to variations in quality control and potential interactions with modern medications.
The following sections will detail specific herbal teas known to pose risks during pregnancy, along with the rationale behind their contraindications. Safe alternatives and considerations for consulting healthcare professionals will also be discussed.
Guidance on Selecting Herbal Teas During Pregnancy
The subsequent advice provides critical insights for individuals seeking to navigate the complexities of herbal tea consumption throughout gestation. It emphasizes informed decision-making and prioritization of maternal and fetal health.
Tip 1: Diligently Review Ingredient Lists. Examine the components of any herbal tea product. Substances like pennyroyal, blue cohosh, and mugwort are documented as potentially harmful and should be unequivocally avoided.
Tip 2: Consult with Qualified Healthcare Providers. Prior to incorporating any herbal tea into the prenatal regimen, seek consultation from a physician, midwife, or registered herbalist. These professionals can offer personalized recommendations based on individual medical history and pregnancy status.
Tip 3: Exercise Caution with Proprietary Blends. Exercise heightened vigilance regarding proprietary blends, as the precise ingredients and their concentrations are often undisclosed. Opt for single-herb teas with transparent labeling.
Tip 4: Research Potential Interactions. Understand that certain herbal constituents may interact with prescribed medications or pre-existing medical conditions. Comprehensive research, ideally guided by a healthcare provider, is imperative.
Tip 5: Limit Consumption of High-Risk Herbs in Other Forms. Recognize that herbs present in teas may also be found in supplements or other products. Scrutinize all consumed items for potentially harmful ingredients.
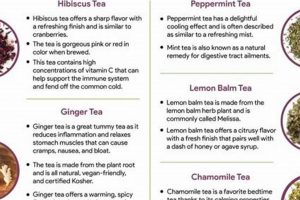
Tip 6: Prioritize Known Safe Options. Focus on herbal teas widely recognized as safe for pregnancy, such as chamomile, ginger (in moderation), and red raspberry leaf (with provider approval and in later trimesters). Thoroughly research each herb’s appropriate use.
Tip 7: Source Herbal Teas from Reputable Suppliers. Ensure that purchased herbal teas originate from reputable sources that adhere to stringent quality control standards and provide accurate product information.
Adhering to these guidelines enables individuals to make informed choices, minimizing the potential for adverse effects associated with certain herbal teas during pregnancy. The emphasis remains on prioritizing maternal and fetal well-being through knowledge and careful consideration.
The article will next address safe herbal tea alternatives and provide further context for making informed decisions during pregnancy.
1. Uterine Stimulation
Uterine stimulation, in the context of herbal teas to avoid during pregnancy, refers to the capacity of certain herbal constituents to induce or intensify contractions of the uterine muscles. This effect presents a potential risk to the pregnancy, particularly during the early trimesters when the uterine lining is still establishing and maintaining a secure environment for fetal development.
- Oxytocic Effects
Some herbs contain compounds that mimic or enhance the effects of oxytocin, a hormone responsible for stimulating uterine contractions during labor. In pregnancy, premature or excessive oxytocic activity can lead to uterine cramping, spotting, or, in severe cases, miscarriage. Examples include herbs traditionally used to induce labor, such as blue cohosh and black cohosh.
- Prostaglandin Production
Certain herbal constituents can stimulate the production of prostaglandins, hormone-like substances that play a role in inflammation and smooth muscle contraction, including in the uterus. Increased prostaglandin levels can lead to uterine irritability and contractions. Herbs like evening primrose oil, while sometimes used later in pregnancy under supervision, can pose risks if used inappropriately.
- Direct Myometrial Action
Specific compounds found in certain herbs may directly act on the myometrium, the muscular wall of the uterus, causing it to contract. This mechanism bypasses hormonal pathways and directly affects uterine muscle tone. Pennyroyal, for example, contains pulegone, a compound known to stimulate uterine contractions and should be strictly avoided.
- Increased Uterine Blood Flow
While increased blood flow can be beneficial in certain contexts, some herbs can excessively increase uterine blood flow, potentially leading to complications during pregnancy. This overstimulation can disrupt the delicate balance needed for maintaining a healthy pregnancy and may exacerbate existing uterine sensitivities. Certain strong circulatory stimulants should be used cautiously, if at all.
The connection between uterine stimulation and herbal teas highlights the importance of thorough research and professional consultation. Herbal teas containing substances known to stimulate uterine activity should be strictly avoided during pregnancy to minimize the risk of adverse outcomes. The potential for adverse effects necessitates a cautious approach to herbal consumption during gestation.
2. Hormonal disruption
Hormonal disruption, in the context of herbal teas consumed during pregnancy, denotes the interference with the complex endocrine system that governs reproductive processes. Specific herbal constituents possess the capacity to mimic, block, or otherwise alter the production, metabolism, or action of key hormones, such as estrogen, progesterone, and human chorionic gonadotropin (hCG). Given the critical role of these hormones in maintaining pregnancy, disruption can lead to adverse outcomes.
Certain herbal teas contain phytoestrogens, compounds structurally similar to estrogen, which can bind to estrogen receptors and exert estrogenic or anti-estrogenic effects. While mild estrogenic activity may be inconsequential in non-pregnant individuals, in pregnancy, it can potentially disrupt the delicate hormonal balance required for uterine receptivity and placental function. Examples include teas containing high concentrations of licorice root or red clover. Other herbs may interfere with progesterone production or signaling, which is essential for maintaining the uterine lining and preventing preterm labor. Vitex (chasteberry), though often used to regulate menstrual cycles, should be avoided during pregnancy due to its potential to affect prolactin and progesterone levels.
The understanding of hormonal disruption caused by herbal teas is of practical significance. Pregnant individuals should diligently scrutinize ingredient lists and consult healthcare providers before consuming any herbal tea. Avoiding teas with known hormonal activity, particularly those containing phytoestrogens or those purported to affect menstrual cycles, is a prudent strategy. A cautious approach, prioritizing evidence-based recommendations, is essential to mitigating potential risks associated with hormonal disruption during pregnancy.
3. Emmenagogue effects
Emmenagogue effects, pertaining to herbal teas, are crucial considerations during gestation. These effects involve the capacity of certain herbs to stimulate or increase menstrual flow, which can pose significant risks to a developing pregnancy. Understanding this action is paramount when evaluating the safety of herbal teas for pregnant individuals.
- Stimulation of Uterine Contractions
Many herbs with emmenagogue properties achieve their effect by stimulating uterine contractions. This stimulation can range from mild cramping to strong contractions capable of disrupting the uterine lining and potentially leading to miscarriage, particularly during early pregnancy. Pennyroyal and mugwort are examples of herbs known to induce such contractions and are contraindicated during pregnancy.
- Increased Pelvic Blood Flow
Emmenagogue herbs often promote increased blood flow to the pelvic region, including the uterus. While increased blood flow can be beneficial in non-pregnant states for addressing menstrual irregularities, it poses a risk during pregnancy by potentially destabilizing the uterine environment and leading to bleeding or placental disruption. Herbs like rue and tansy are known to have this effect.
- Hormonal Influence
Some emmenagogue herbs exert their effects by influencing hormonal balance, particularly impacting estrogen and progesterone levels. These hormonal shifts can disrupt the delicate hormonal milieu required for maintaining pregnancy, potentially leading to complications. Herbs such as black cohosh, while used for menopausal symptoms, can have significant hormonal effects and should be avoided.
- Potential for Fetal Harm
Beyond direct effects on the uterus, some emmenagogue herbs contain compounds that can be directly toxic to the developing fetus. These compounds can cross the placental barrier and interfere with fetal development, leading to birth defects or fetal demise. Herbs like savin are examples of those that contain toxic compounds and must be strictly avoided.
The emmenagogue properties of certain herbs underscore the importance of caution when selecting herbal teas during pregnancy. The potential for uterine stimulation, increased pelvic blood flow, hormonal influence, and direct fetal harm necessitates a thorough evaluation of all herbal ingredients and consultation with qualified healthcare professionals. Failure to recognize and avoid these effects can have serious consequences for both maternal and fetal health.
4. Toxicity potential
The toxicity potential of certain herbal teas presents a direct contraindication during pregnancy. Specific plant constituents, when ingested, can exhibit adverse effects on maternal and fetal health, ranging from mild discomfort to severe developmental abnormalities or pregnancy loss. This potential toxicity stems from inherent chemical properties of the herbs themselves, which may interfere with essential physiological processes or directly harm developing fetal tissues. The determination of toxicity potential is a critical component in identifying herbal teas to avoid when pregnant. For example, pennyroyal contains pulegone, a volatile oil known to cause liver damage and induce abortions, illustrating the direct link between a specific chemical constituent and adverse pregnancy outcomes. Similarly, excessive consumption of licorice root, even outside of pregnancy, can lead to pseudoaldosteronism, but in pregnancy, it raises concerns about fetal development and potential preterm labor due to its glycyrrhizin content.
The manifestation of toxicity can vary depending on the specific herb, dosage, and gestational stage. In the first trimester, when organogenesis is occurring, exposure to toxic compounds can disrupt cellular differentiation and lead to congenital anomalies. Later in pregnancy, such exposure may affect fetal growth and development, or even induce premature labor. Understanding the toxicity potential involves considering both the acute and chronic effects of herbal constituents. Acute toxicity refers to immediate adverse reactions, while chronic toxicity concerns the cumulative effects of prolonged exposure to lower doses. Some herbs, considered safe in small amounts, may become toxic when consumed regularly or in larger quantities. Therefore, risk assessment requires consideration of both the concentration of toxic compounds and the frequency of consumption.
In conclusion, the toxicity potential of herbal teas represents a significant consideration during pregnancy due to the direct threat posed to maternal and fetal well-being. Recognizing the specific herbs with known toxic constituents, understanding their mechanisms of action, and avoiding their consumption are crucial steps in ensuring a safe pregnancy. The challenges lie in the variability of herbal products, the lack of standardized dosage information, and the limited research specifically addressing pregnancy outcomes. This underscores the importance of consulting healthcare professionals and exercising caution when considering any herbal tea during pregnancy, prioritizing evidence-based recommendations over anecdotal information.
5. Fetal harm
Fetal harm, in the context of herbal teas to avoid during pregnancy, constitutes the most severe potential consequence of maternal ingestion. This encompasses a spectrum of adverse outcomes, ranging from subtle developmental disruptions to severe congenital malformations, pregnancy loss, or even fetal death. The connection between specific herbal constituents and fetal harm arises from the capacity of these compounds to cross the placental barrier and directly interfere with critical processes of fetal development. For example, certain alkaloids present in herbs like pennyroyal can cause liver damage and neurotoxicity in the developing fetus, while others may disrupt essential hormonal pathways, leading to irreversible developmental abnormalities. The importance of understanding this connection cannot be overstated, as it directly impacts the decisions expectant mothers make regarding their dietary choices.
The manifestation of fetal harm is contingent upon several factors, including the specific herb consumed, the dosage, the gestational stage at the time of exposure, and the individual susceptibility of the fetus. During the first trimester, when organogenesis is actively occurring, exposure to teratogenic herbal constituents poses the greatest risk of structural malformations. Later in pregnancy, exposure may primarily affect fetal growth, neurological development, or organ maturation. Furthermore, some herbal teas may indirectly cause fetal harm by inducing uterine contractions, placental abruption, or other maternal complications that compromise fetal well-being. For example, certain herbal teas with strong emmenagogue properties, such as mugwort, can stimulate uterine bleeding and potentially lead to miscarriage, especially in early pregnancy. The practical significance of this understanding lies in the imperative to avoid herbal teas with known or suspected teratogenic or abortifacient properties during pregnancy. This requires careful scrutiny of product labels, consultation with healthcare professionals, and a cautious approach to herbal remedies in general.
In conclusion, fetal harm represents the most serious adverse outcome associated with the consumption of certain herbal teas during pregnancy. The potential for direct toxicity, developmental disruption, or pregnancy complications underscores the critical importance of informed decision-making and avoidance of potentially harmful herbal constituents. Challenges remain in fully elucidating the risks associated with all herbal products, due to limited research and standardization. Therefore, a conservative approach, guided by evidence-based recommendations and professional medical advice, is essential to safeguarding fetal health and ensuring a successful pregnancy. The ultimate goal is to minimize any potential exposure to substances that could compromise the well-being of the developing fetus, prioritizing a healthy pregnancy outcome.
6. Insufficient research
The category of herbal teas to avoid during pregnancy is significantly informed by a lack of comprehensive scientific investigation. The absence of robust clinical trials specifically evaluating the safety and efficacy of many herbal constituents during gestation necessitates a precautionary approach. This deficiency in research creates uncertainty regarding potential teratogenic effects, impacts on uterine contractility, and hormonal disruptions, leading to the classification of certain herbal teas as potentially hazardous for pregnant individuals. The cause-and-effect relationship is evident: limited data prevents a definitive safety assessment, resulting in avoidance recommendations. Insufficient research is, therefore, not merely a peripheral consideration but a core determinant in identifying “herbal teas to avoid when pregnant”. For example, while anecdotal evidence may suggest traditional uses for certain herbs, without rigorous scientific validation, their safety profile remains questionable. The limited research on chamomile, compared to pennyroyal, allows for its more widespread acceptance during pregnancy, albeit still with caveats. The practical significance of recognizing this research gap lies in understanding that avoidance is often based on the absence of evidence proving safety, rather than definitive evidence of harm.
This scarcity of data stems from ethical and logistical challenges in conducting research on pregnant women. The potential risks to the fetus necessitate extreme caution, making it difficult to justify randomized controlled trials involving potentially harmful substances. Furthermore, the variability in herbal preparations, including differences in growing conditions, harvesting methods, and processing techniques, adds complexity to research design and interpretation. The absence of standardized dosages and formulations further complicates the development of evidence-based guidelines. The practical application of this understanding involves a heightened awareness of the limitations of available information and a reliance on conservative recommendations. Healthcare providers must often rely on in vitro studies, animal models, and case reports to inform their guidance, recognizing that these sources may not fully translate to human pregnancy.
In conclusion, insufficient research is a critical factor influencing the classification of herbal teas to avoid during pregnancy. The ethical and logistical challenges in conducting research on pregnant women contribute to the scarcity of data, resulting in uncertainty regarding the safety of many herbal constituents. This lack of definitive evidence necessitates a cautious approach, emphasizing avoidance based on the absence of proven safety. Addressing this challenge requires further investment in alternative research methodologies, such as large-scale observational studies and rigorous analysis of existing data. Until more comprehensive research is available, pregnant individuals should prioritize evidence-based recommendations and consult with healthcare professionals to make informed decisions regarding herbal tea consumption, mitigating potential risks to maternal and fetal well-being.
Frequently Asked Questions
This section addresses common inquiries and clarifies potential misconceptions regarding the selection of herbal teas during pregnancy. The goal is to provide accurate information to promote informed decision-making.
Question 1: Why are some herbal teas considered unsafe during pregnancy?
Certain herbal teas contain constituents with potential teratogenic, abortifacient, or hormonally disruptive effects. These constituents can cross the placental barrier, potentially harming the developing fetus or disrupting the pregnancy itself.
Question 2: How can individuals determine if an herbal tea is safe for consumption during pregnancy?
Careful examination of the ingredient list is essential. Any tea containing herbs known to be contraindicated during pregnancy (e.g., pennyroyal, blue cohosh) should be avoided. Consultation with a qualified healthcare provider or registered herbalist is strongly recommended.
Question 3: Is “natural” always synonymous with “safe” in the context of herbal teas during pregnancy?
No. The term “natural” does not guarantee safety. Many naturally occurring substances can be harmful or even toxic, particularly during sensitive periods such as pregnancy. A critical evaluation of the specific herbal ingredients is necessary.
Question 4: Are small amounts of unsafe herbal teas permissible during pregnancy?
Due to the potential for cumulative effects and individual sensitivities, even small amounts of herbal teas known to be unsafe should be avoided. There is no established safe threshold for many contraindicated herbs.
Question 5: Can herbal teas interact with prescription medications during pregnancy?
Yes. Certain herbal constituents can interact with prescription medications, potentially altering their efficacy or increasing the risk of adverse side effects. Healthcare providers should be informed of all herbal supplements and teas being consumed.
Question 6: What are some reliably safe herbal tea options during pregnancy?
Some herbal teas generally considered safe in moderation during pregnancy include chamomile, ginger (for nausea relief), and red raspberry leaf (typically in later trimesters and with healthcare provider approval). However, individual tolerances and medical conditions should always be considered, and consultation with a healthcare provider remains essential.
The key takeaway is that the safety of herbal teas during pregnancy necessitates careful consideration and professional guidance. Erroneous assumptions based solely on anecdotal evidence or marketing claims should be avoided. Prioritizing informed decision-making is crucial.
The following section will further delve into safe herbal tea alternatives, offering practical guidance for those seeking suitable beverage options during pregnancy.
Herbal Teas to Avoid When Pregnant
This examination of “herbal teas to avoid when pregnant” has underscored the potential risks associated with certain plant-based infusions during gestation. Key concerns include uterine stimulation, hormonal disruption, emmenagogue effects, toxicity potential, fetal harm, and the pervasive issue of insufficient research to guarantee safety. The information presented serves as a guide, emphasizing the necessity of informed decision-making and professional consultation.
Given the complexities inherent in herbal medicine and the vulnerability of the developing fetus, a cautious approach is paramount. The responsibility lies with individuals and healthcare providers to prioritize evidence-based recommendations and mitigate potential risks. Continued vigilance and further research remain essential to refine our understanding and ensure optimal pregnancy outcomes.