The practice of using botanical remedies to stimulate the commencement of childbirth is a long-standing tradition in various cultures. These methods encompass a range of plant-derived substances believed to encourage uterine contractions and cervical ripening. A typical example involves the consumption of specific herbs or the application of herbal preparations to promote the onset of labor.
Historically, the appeal of such approaches stems from their accessibility and perceived naturalness. Advocates suggest potential advantages such as greater control over the birthing process and avoidance of pharmaceutical interventions. Furthermore, in certain communities, these practices are deeply intertwined with cultural beliefs and traditional medicinal systems, representing a significant aspect of maternal healthcare.
The subsequent discussion will delve into the specifics of commonly employed botanicals, explore the evidence regarding their efficacy and safety, and address critical considerations for healthcare providers and expectant mothers evaluating these options.
Guidance on the Use of Botanicals to Initiate Childbirth
The following points provide important considerations when exploring the potential use of plant-derived substances to encourage the onset of labor.
Tip 1: Consult a Qualified Healthcare Provider: Prior to considering any botanical method, a comprehensive discussion with a physician or midwife is essential. This consultation should involve a thorough assessment of the individual’s medical history, pregnancy status, and potential risks.
Tip 2: Understand Potential Risks: Botanical substances can have potent physiological effects, potentially leading to adverse outcomes for both mother and fetus. Risks may include uterine hyperstimulation, fetal distress, and allergic reactions. A full awareness of the potential risks involved is critical before proceeding.
Tip 3: Research the Evidence Base: The scientific evidence supporting the effectiveness and safety of many botanical labor induction methods is limited. A critical evaluation of available research, considering study design and limitations, is necessary.
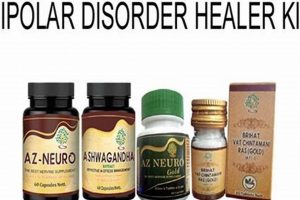
Tip 4: Source Botanicals Responsibly: The quality and purity of botanical products can vary significantly. It is crucial to obtain products from reputable sources that adhere to quality control standards. Adulteration and misidentification are potential concerns.
Tip 5: Be Aware of Dosage and Preparation: Accurate dosing and proper preparation methods are essential to minimize potential adverse effects. Follow established protocols and guidelines carefully. Consult with a knowledgeable herbalist or healthcare professional for guidance.
Tip 6: Monitor for Side Effects: Close monitoring for any adverse reactions is crucial throughout the process. Discontinue use and seek immediate medical attention if any concerning symptoms develop.
Tip 7: Have a Backup Plan: If botanical methods are unsuccessful in initiating labor, a plan for conventional medical induction should be in place. This ensures timely and appropriate intervention when necessary.
Careful consideration of these points is essential to promoting informed decision-making and minimizing potential risks when contemplating the use of botanicals to initiate childbirth.
The subsequent sections will explore alternative approaches and provide further context regarding the overall management of pregnancy and labor.
1. Safety Concerns
The utilization of botanical substances to initiate childbirth introduces significant safety considerations that demand careful scrutiny. Given the potential for potent physiological effects on both the pregnant individual and the fetus, a thorough evaluation of risks is paramount.
- Uterine Hyperstimulation
Some botanical agents are believed to stimulate uterine contractions. However, excessive or uncoordinated contractions can lead to uterine hyperstimulation, potentially compromising fetal oxygen supply and increasing the risk of uterine rupture, especially in individuals with prior cesarean deliveries. Vigilant monitoring of contraction patterns is essential to mitigate this risk.
- Fetal Distress
Compromised uteroplacental blood flow resulting from uterine hyperstimulation or other adverse effects of botanical agents can induce fetal distress. Signs of fetal distress may include abnormal fetal heart rate patterns, decreased fetal movement, or meconium-stained amniotic fluid. Prompt intervention, including potential cessation of the botanical agent and medical management, is crucial in such cases.
- Adverse Maternal Effects
Botanical substances may elicit a range of adverse effects in the pregnant individual, including gastrointestinal upset, allergic reactions, changes in blood pressure, and alterations in coagulation. The severity of these effects can vary depending on the specific agent used, the individual’s susceptibility, and the dosage administered. Careful monitoring for any signs of adverse reactions is essential.
- Lack of Standardized Products
The absence of standardized manufacturing processes and quality control measures for many botanical products poses a significant safety concern. Variations in potency, purity, and adulteration can lead to unpredictable effects and increase the risk of adverse outcomes. Obtaining products from reputable sources and verifying their composition is critical to minimize this risk.
These safety concerns underscore the need for a cautious and evidence-based approach to utilizing botanical methods for initiating childbirth. Comprehensive risk assessment, informed consent, close monitoring, and access to conventional medical care are essential components of responsible practice.
2. Efficacy evidence
The demonstrable effectiveness of botanicals in initiating childbirth remains a complex and often contentious area. A direct causal relationship between the administration of a specific herb and the onset of labor is frequently difficult to establish due to the multifactorial nature of labor itself and the inherent challenges in conducting rigorous clinical trials. The variability in botanical preparations, dosage, and individual physiological responses further complicates the assessment of true efficacy. The reliance on anecdotal accounts or traditional usage, while providing historical context, does not constitute sufficient evidence to support widespread adoption. For instance, while some studies suggest a possible association between evening primrose oil and cervical ripening, robust, placebo-controlled trials are often lacking, making it challenging to definitively attribute labor onset to this specific botanical.
The importance of robust efficacy evidence stems from ethical considerations and the need to ensure patient safety. If a botanical intervention lacks demonstrable effectiveness, its use may delay access to more reliable and evidence-based medical interventions, potentially increasing risks for both mother and fetus. Furthermore, ineffective interventions can undermine trust in healthcare providers and the broader medical system. The practical significance of understanding the limits of efficacy evidence lies in fostering realistic expectations and promoting informed decision-making. Expectant mothers should be fully aware of the potential benefits and risks, including the possibility that a botanical approach may not be successful in initiating labor and that alternative medical interventions may ultimately be necessary. For example, a woman attempting to initiate labor with blue cohosh should be informed that its effectiveness is not well-established and that its use carries potential cardiovascular risks for the newborn.
In conclusion, the relationship between efficacy evidence and botanical interventions for initiating childbirth is characterized by a need for more rigorous scientific investigation. While historical usage and anecdotal experiences may provide a basis for exploration, robust clinical trials are essential to determine true efficacy and safety. Until such evidence is available, a cautious and evidence-based approach, prioritizing patient safety and informed decision-making, is paramount. Challenges persist in standardizing botanical preparations and accounting for individual physiological variations, but continued research is necessary to clarify the potential role, if any, of these interventions in modern obstetric care.
3. Qualified guidance
The practice of using plant-derived substances to encourage the commencement of childbirth necessitates competent oversight to mitigate potential risks and promote informed decision-making. Competent direction, in this context, involves the integration of medical expertise, pharmacological knowledge, and an understanding of individual patient circumstances.
- Medical Risk Assessment
A qualified healthcare provider can conduct a thorough assessment of the individual’s medical history, pregnancy status, and potential contraindications to botanical agents. For example, a woman with a history of uterine surgery may be at increased risk of uterine rupture with certain herbs, and a qualified practitioner can identify this risk. The medical risk assessment ensures that botanical interventions are only considered when the potential benefits outweigh the risks.
- Pharmacological Expertise
A knowledgeable professional possesses an understanding of the pharmacological properties of various herbs, including their mechanisms of action, potential drug interactions, and adverse effects. For instance, certain herbs may interact with anticoagulants or antihypertensive medications, potentially leading to serious complications. Pharmacological expertise is essential for selecting appropriate agents and avoiding harmful interactions.
- Dosage and Preparation Guidance
Accurate dosing and proper preparation methods are critical to minimizing the risk of adverse effects and maximizing the potential benefits of botanical interventions. A qualified expert can provide guidance on appropriate dosages based on individual factors and ensure that herbs are prepared correctly to maintain their potency and purity. For example, the method of preparing a herbal tea (infusion vs decoction) can alter its strength and potential effects.
- Monitoring and Intervention
A skilled healthcare provider can monitor the pregnant individual for any signs of adverse reactions or complications during the course of botanical intervention. This includes monitoring uterine contraction patterns, fetal heart rate, and maternal vital signs. The ability to recognize and respond to potential complications is essential for ensuring the safety of both mother and fetus. For example, if uterine hyperstimulation occurs, a qualified practitioner can administer medications to relax the uterus and prevent fetal distress.
The integration of these facets underscores the crucial role of competent direction in the practice of using botanical substances to initiate childbirth. Without knowledgeable supervision, the potential risks associated with these interventions may outweigh their benefits, potentially compromising maternal and fetal well-being. Therefore, seeking guidance from qualified healthcare professionals is paramount when considering botanical methods to initiate childbirth.
4. Dosage accuracy
Dosage accuracy is a critical determinant of both the safety and efficacy of botanical interventions intended to initiate childbirth. Deviations from recommended dosages can lead to adverse maternal and fetal outcomes, ranging from ineffective treatment to severe complications. The inherent variability in botanical preparations further underscores the importance of precise dosing.
- Variable Potency of Herbal Products
The concentration of active compounds can vary significantly between different batches of the same herb due to factors such as growing conditions, harvesting methods, and processing techniques. This variability makes it challenging to determine a standardized dose, and inaccurate dosing can result in either sub-therapeutic effects or toxic reactions. For instance, one batch of black cohosh may contain significantly more of the active constituents than another, leading to inconsistent effects if the same dosage is used.
- Individual Physiological Variability
Individual differences in metabolism, body weight, and sensitivity to herbal compounds influence how a person responds to a given dose. Factors such as liver function, kidney function, and pre-existing medical conditions can affect the absorption, distribution, metabolism, and excretion of herbal constituents. Therefore, a dosage that is safe and effective for one individual may be ineffective or harmful for another. For example, a smaller individual may require a lower dose of blue cohosh compared to a larger individual to achieve the desired effect without experiencing adverse cardiovascular effects.
- Potential for Drug Interactions
Herbal substances can interact with conventional medications, either enhancing or diminishing their effects. Inaccurate dosing can exacerbate these interactions, leading to unpredictable and potentially dangerous outcomes. For example, excessive consumption of herbs with anticoagulant properties in combination with prescription blood thinners can increase the risk of bleeding. Precise dosage management is essential to minimize the risk of adverse drug interactions.
- Importance of Standardization and Quality Control
Standardization of herbal products and rigorous quality control measures are crucial for ensuring dosage accuracy. Standardized extracts contain a consistent concentration of active compounds, allowing for more precise dosing. However, many herbal products are not standardized, making it difficult to determine the appropriate dosage. Quality control measures, such as testing for contaminants and verifying the identity of the herb, are also essential for ensuring product safety and efficacy. Consumers should seek out products that have been independently tested and certified to ensure quality and dosage accuracy.
The inherent challenges in achieving dosage accuracy with botanical agents highlight the need for a cautious and informed approach. Comprehensive medical assessment, qualified guidance, and the use of standardized products, when available, are essential to minimize the risks and maximize the potential benefits of using plant-derived substances to initiate childbirth.
5. Source credibility
The reliability of information pertaining to botanical methods intended to initiate childbirth is paramount due to the potential risks involved. The source from which such information originates directly impacts the validity of claims made regarding efficacy, safety, and appropriate usage. Unverified sources, lacking in scientific rigor or medical oversight, can disseminate inaccurate or incomplete information, leading to inappropriate or harmful practices. For example, anecdotal accounts on unregulated online forums may promote the use of specific herbs without acknowledging potential contraindications or interactions with existing medical conditions. Conversely, information derived from peer-reviewed medical journals, reputable healthcare organizations, or qualified herbalists with verifiable credentials holds significantly greater weight. The cause-and-effect relationship is clear: reliance on credible sources promotes safe and informed decision-making, while dependence on unreliable sources elevates the risk of adverse outcomes.
The importance of source credibility is further underscored by the variability in botanical products available to consumers. The purity, potency, and even the correct identification of herbs can differ significantly depending on the manufacturer and supplier. Reputable sources adhere to stringent quality control standards, ensuring that products are accurately labeled, free from contaminants, and contain the stated concentration of active compounds. Conversely, unregulated sources may offer adulterated or misidentified products, posing serious health risks. A real-life example is the substitution of authentic goldenseal with cheaper, but less effective, substitutes. Distinguishing between credible and unreliable sources necessitates careful evaluation of the provider’s credentials, manufacturing processes, and quality control measures.
In conclusion, source credibility forms an indispensable component of the responsible use of botanical substances to initiate childbirth. The challenges associated with verifying the accuracy and reliability of information emphasize the need for a discerning approach. By prioritizing information from reputable healthcare providers, evidence-based resources, and qualified herbalists, individuals can make informed decisions that minimize risks and promote maternal and fetal well-being. This understanding is of practical significance, guiding expectant parents towards safer, more effective choices within the realm of complementary and alternative medicine.
6. Cultural context
The use of botanical methods to initiate childbirth is frequently interwoven with specific cultural traditions and belief systems. These practices, passed down through generations, represent an integral part of maternal healthcare within certain communities. The rationale for utilizing specific herbs, the preparation methods employed, and the rituals surrounding their administration are often deeply rooted in cultural narratives and understandings of female reproductive health. This cultural context influences both the perceived efficacy and the acceptance of these methods within the community. For example, certain indigenous cultures may view labor as a natural process best supported by traditional herbal remedies administered by experienced midwives, a perspective that shapes their approach to childbirth significantly.
The importance of cultural context extends to understanding the potential risks and benefits associated with specific botanical practices. What may be considered a safe and effective remedy within one cultural group may be viewed with skepticism or even considered harmful in another. This variance arises from differences in plant knowledge, preparation techniques, and the physiological understanding of the substances involved. For instance, the use of castor oil to induce labor is a practice common in some cultures, while others may discourage it due to concerns about potential complications. Awareness of these cultural nuances is crucial for healthcare providers interacting with patients from diverse backgrounds, allowing for culturally sensitive communication and collaborative decision-making.
A comprehensive understanding of cultural context is essential for promoting equitable and respectful maternal healthcare. This knowledge enables healthcare providers to engage in meaningful dialogue with patients about their beliefs and preferences regarding labor and delivery, fostering a collaborative approach that respects cultural traditions while ensuring patient safety. Ignoring the cultural dimensions of botanical induction practices can lead to misunderstandings, mistrust, and potentially adverse health outcomes. Therefore, recognizing and respecting the cultural context is not only ethically imperative but also practically significant for achieving optimal maternal and neonatal well-being.
Frequently Asked Questions
The following questions and answers address common inquiries and concerns surrounding the use of botanical substances to stimulate the commencement of childbirth. This information is intended for educational purposes and should not be construed as medical advice.
Question 1: Is herbal induction of labor a safe alternative to conventional medical induction?
The safety profile of botanical induction methods is generally less well-established compared to conventional medical induction. While some herbs are perceived as “natural,” they can still possess potent physiological effects and carry potential risks for both the pregnant individual and the fetus. Conventional medical induction methods are typically subject to rigorous clinical trials and regulatory oversight.
Question 2: What are the potential risks associated with herbal induction of labor?
Risks may include uterine hyperstimulation, fetal distress, adverse maternal reactions (e.g., allergic reactions, gastrointestinal upset), and a lack of standardized dosing, leading to unpredictable effects. The use of certain herbs may also be contraindicated in individuals with specific medical conditions or pregnancy complications.
Question 3: Is there scientific evidence to support the effectiveness of herbal induction of labor?
The scientific evidence supporting the effectiveness of many botanical labor induction methods is limited. While some studies suggest potential benefits for certain herbs, many of these studies are small, lack rigorous controls, or suffer from methodological limitations. More research is needed to determine the true efficacy and safety of these interventions.
Question 4: Can any herbal substance be used to initiate labor?
No. Not all herbal substances are safe or appropriate for use during pregnancy. Certain herbs are known to be contraindicated due to their potential to cause harm to the mother or fetus. It is crucial to consult with a qualified healthcare provider or experienced herbalist before using any botanical substance to initiate labor.
Question 5: What should be done if herbal induction methods are unsuccessful?
If botanical methods are unsuccessful in initiating labor within a reasonable timeframe, a plan for conventional medical induction should be in place. Prolonged attempts at herbal induction may delay access to more reliable interventions and potentially increase risks for both mother and fetus.
Question 6: Where can reliable information about herbal induction of labor be found?
Reliable information can be obtained from qualified healthcare providers, evidence-based medical resources (e.g., medical journals, professional organizations), and experienced herbalists with verifiable credentials. Information from unregulated online sources should be approached with caution.
In summary, the use of herbal substances to initiate childbirth carries both potential benefits and risks. A cautious and informed approach, guided by qualified healthcare professionals, is essential to ensuring maternal and fetal safety.
The following section will explore legal and ethical considerations related to this practice.
Conclusion
The preceding analysis has explored the multifaceted nature of using botanical substances to stimulate the commencement of childbirth. Key considerations include the limited scientific evidence supporting efficacy, the potential safety risks associated with unregulated use, and the importance of qualified guidance in navigating these complexities. Cultural contexts play a significant role in shaping perceptions and practices, while dosage accuracy and source credibility remain paramount to minimizing potential harm.
Given the inherent uncertainties and potential risks associated with herbal induction of labor, expectant mothers and healthcare providers are urged to prioritize evidence-based decision-making and informed consent. Further research is warranted to fully elucidate the safety and efficacy profiles of specific botanical agents, ensuring that any utilization of these methods is grounded in robust scientific evidence and aligned with best practices in maternal healthcare.