This refers to the concept of utilizing plant-derived remedies as a substitute for conventional pharmaceutical interventions when addressing health concerns, with a particular focus on those explored or influenced by traditional practices and knowledge stemming from regions historically connected to, or impacted by, figures like Hernn Corts. It involves investigating and employing botanical resources believed to possess therapeutic properties, aiming to alleviate symptoms or promote well-being through natural means rather than synthetic drugs. For instance, certain indigenous plant extracts might be considered for managing inflammation or supporting immune function.
The significance of this approach lies in its potential to offer gentler, more holistic avenues for health management, often with fewer reported side effects compared to synthetic pharmaceuticals. Historically, communities in various regions have relied on local flora for medicinal purposes, accumulating a wealth of knowledge regarding their properties and applications. This legacy continues to inform modern research and practice, highlighting the enduring relevance of botanical medicine in addressing a range of ailments and fostering overall health.
The subsequent sections will delve deeper into specific plant species, their purported therapeutic effects, and the scientific evidence supporting their use. Furthermore, it will examine the potential risks and benefits associated with incorporating such alternatives into a health regimen and the need for consultation with qualified healthcare professionals to ensure safe and effective application.
Guidance on Plant-Based Substitute Methods
The following recommendations provide a framework for navigating the responsible exploration of plant-based substitute methods. These guidelines prioritize safety, efficacy, and informed decision-making.
Tip 1: Research Thoroughly: Before incorporating any plant-derived substance, conduct extensive research. Consult reputable sources such as peer-reviewed journals, academic publications, and established herbal medicine databases to understand the plant’s properties, potential benefits, and known risks.
Tip 2: Consult with a Qualified Healthcare Professional: Engage with a physician, naturopathic doctor, or herbalist experienced in botanical medicine. This professional can assess individual health needs, identify potential interactions with existing medications, and provide personalized recommendations.
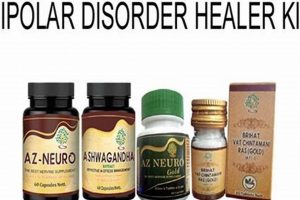
Tip 3: Identify Reliable Sources: Purchase plant-based products from reputable suppliers who adhere to quality control standards. Verify that products are properly identified, tested for contaminants, and accurately labeled with ingredient information and dosage instructions.
Tip 4: Start with Low Doses: When introducing a new botanical substance, begin with a low dose to assess individual tolerance. Gradually increase the dosage as directed by a healthcare professional, while closely monitoring for any adverse reactions.
Tip 5: Be Aware of Potential Interactions: Recognize that plant-derived substances can interact with conventional medications, dietary supplements, and even certain foods. Disclose all current medications and supplements to a healthcare professional to prevent potentially harmful interactions.
Tip 6: Monitor for Adverse Reactions: Pay close attention to any changes in health or well-being after incorporating a plant-based substance. Discontinue use immediately and seek medical attention if experiencing allergic reactions, digestive upset, skin rashes, or other concerning symptoms.
Tip 7: Practice Sustainable Sourcing: Support environmentally responsible practices by choosing products derived from sustainably harvested or cultivated plants. This helps to protect biodiversity and ensure the long-term availability of these valuable resources.
These considerations emphasize the importance of informed and responsible engagement with plant-based substitute options. Prioritizing safety and professional guidance can maximize potential benefits while minimizing risks.
The article will now transition to discussing ethical considerations related to resource utilization and the preservation of traditional botanical knowledge.
1. Geographical Origins
The geographical origin of a plant significantly impacts its chemical composition and, consequently, its suitability as a plant-based substitute. Environmental factors such as soil composition, climate, and altitude influence the production of secondary metabolites, which are often responsible for the plant’s therapeutic properties. Thus, the same plant species grown in different regions may exhibit variations in its chemical profile, affecting its efficacy and potential toxicity. Understanding these geographical nuances is crucial for ensuring consistent quality and predictable effects when utilizing botanicals.
For example, consider the use of Artemisia annua (sweet wormwood), a source of artemisinin, a potent antimalarial compound. While this plant can be cultivated in various regions, the artemisinin content can vary significantly depending on factors like soil nutrients and rainfall. This variation can lead to inconsistencies in the effectiveness of Artemisia annua-based treatments, highlighting the need for sourcing from regions known to produce plants with consistently high concentrations of the desired bioactive compounds. Moreover, indigenous knowledge often ties specific plant uses to particular locations, reflecting an understanding of these geographical nuances.
In summary, the geographical origin of a plant is not merely a matter of location but a critical determinant of its therapeutic potential and safety. Identifying reliable sources that consider these geographical factors is essential for realizing the benefits while mitigating the risks associated with plant-based substitutions. The influence of location underscores the importance of standardized cultivation practices and rigorous quality control to ensure the efficacy and safety of botanical medicines, irrespective of their origin.
2. Traditional Knowledge
Traditional knowledge, in the context of plant-based alternatives, represents the accumulated wisdom and practical experience of indigenous and local communities regarding the use of plants for medicinal and therapeutic purposes. This body of knowledge, often transmitted orally across generations, provides valuable insights into the properties, preparation methods, and applications of various plant species.
- Identification and Classification
Traditional knowledge systems often include detailed methods for identifying and classifying plants based on morphological characteristics, habitat preferences, and perceived medicinal properties. This allows communities to distinguish between species with similar appearances but different therapeutic effects. For example, indigenous communities in the Amazon basin possess intricate knowledge of the various Banisteriopsis species used in ayahuasca preparations, enabling them to differentiate between plants with varying levels of psychoactive compounds. The correct identification is paramount in ensuring safety and achieving the desired therapeutic outcome.
- Preparation and Formulation Techniques
Traditional knowledge encompasses diverse preparation and formulation techniques aimed at optimizing the extraction and bioavailability of bioactive compounds. These techniques can involve drying, grinding, maceration, decoction, infusion, fermentation, and combinations thereof. For instance, traditional Chinese medicine employs complex decoction methods to extract specific compounds from multiple herbs, creating synergistic formulations tailored to individual patient needs. The knowledge of these techniques is crucial to unlock the full therapeutic potential of plant-based substances.
- Dosage and Administration Guidelines
Traditional knowledge often includes specific guidelines for determining appropriate dosages and routes of administration based on factors such as age, body weight, health condition, and individual sensitivity. These guidelines are often derived from centuries of empirical observation and trial and error. Traditional healers in various cultures may employ different methods for administering herbal remedies, including oral consumption, topical application, inhalation, and bathing. The careful consideration of dosage and administration methods is essential for maximizing efficacy and minimizing potential adverse effects.
- Understanding of Synergistic and Antagonistic Effects
Traditional knowledge frequently recognizes the potential for synergistic and antagonistic interactions between different plant species or between plants and other substances. This understanding allows practitioners to combine plants strategically to enhance therapeutic effects or mitigate potential risks. For example, traditional Ayurvedic medicine utilizes complex herbal formulations containing multiple ingredients that are believed to work synergistically to promote healing and balance. The knowledge of these interactions is vital for creating safe and effective plant-based remedies.
In conclusion, traditional knowledge serves as an invaluable resource for understanding the potential of plant-based substitutions, offering a wealth of information regarding plant identification, preparation, dosage, and potential interactions. While scientific validation is necessary to confirm the efficacy and safety of traditional practices, the integration of traditional knowledge with modern research can lead to the development of more effective and culturally relevant healthcare solutions.
3. Bioactive Compounds
Bioactive compounds are the specific molecules within plants that exert a physiological effect on the human body. In the context of plant-based substitutes, understanding these compounds is paramount to determining efficacy, safety, and potential applications.
- Identification and Characterization
The first step in understanding a plant’s potential lies in identifying and characterizing its bioactive compounds. This process involves advanced analytical techniques such as chromatography and mass spectrometry to isolate and identify individual molecules. For example, the identification of curcuminoids in turmeric (Curcuma longa) has led to extensive research on its anti-inflammatory properties. The chemical structures and properties of these compounds determine their interactions with biological systems.
- Mechanisms of Action
Once identified, the mechanisms of action of bioactive compounds need to be elucidated. This involves studying how these compounds interact with cellular targets, such as enzymes, receptors, and signaling pathways. For instance, the mechanism of action of artemisinin, an antimalarial compound derived from Artemisia annua, involves the formation of free radicals within malaria parasites. Understanding these mechanisms is crucial for predicting therapeutic effects and potential side effects.
- Dosage and Bioavailability
The effectiveness of bioactive compounds depends on their dosage and bioavailability, which refers to the extent to which they are absorbed and utilized by the body. Factors such as solubility, metabolism, and interactions with other compounds can influence bioavailability. For example, the bioavailability of resveratrol, a polyphenol found in grapes and red wine, is limited by its rapid metabolism in the liver. Strategies such as encapsulation or co-administration with other compounds can be employed to enhance bioavailability and improve therapeutic outcomes.
- Safety and Toxicity
Assessment of the safety and toxicity of bioactive compounds is essential to ensure responsible use. This involves conducting preclinical and clinical studies to evaluate potential adverse effects, such as allergic reactions, drug interactions, and organ toxicity. For instance, pyrrolizidine alkaloids, found in some plants, can cause liver damage. Thorough safety evaluation is crucial to minimize risks and ensure that the benefits of plant-based substitutes outweigh potential harms.
The multifaceted understanding of bioactive compounds, from their identification and mechanisms of action to dosage considerations and safety profiles, underpins the rational and evidence-based use of plant-based substitutes. A thorough grasp of these concepts is essential for healthcare professionals and individuals seeking to incorporate these options into their wellness strategies.
4. Dosage Guidelines
Dosage guidelines are a critical component in the responsible utilization of plant-based substitutes, including those conceptually linked to historical or traditional practices from regions impacted by figures such as Hernn Corts. Improper dosage can negate therapeutic benefits and, more seriously, induce adverse effects, ranging from mild discomfort to severe toxicity. Therefore, standardized and evidence-based dosage recommendations are paramount to ensure the safety and efficacy of any botanical intervention. The absence of clear dosage guidelines transforms a potentially beneficial substance into a hazardous one.
The establishment of dosage guidelines for plant-derived remedies is often complex due to several factors. The concentration of active compounds can vary significantly based on plant species, geographical origin, cultivation methods, and preparation techniques. Moreover, individual factors, such as age, weight, health status, and concurrent medication use, can influence a person’s response to a particular dose. Real-world examples illustrate the importance of personalized dosage adjustments. An individual with liver impairment may require a reduced dose of a hepatically metabolized herb compared to a healthy individual to avoid potential toxicity. Similarly, an elderly person may exhibit increased sensitivity to certain botanical substances and necessitate a lower initial dose. Understanding these nuances is not merely academic; it is a matter of patient safety.
In conclusion, the development and adherence to appropriate dosage guidelines are non-negotiable aspects of utilizing plant-based alternatives safely and effectively. The variability in plant composition and individual responses underscores the need for professional guidance from qualified healthcare practitioners who can assess individual needs and provide personalized recommendations. This conscientious approach minimizes the risk of adverse effects and maximizes the potential therapeutic benefits of these traditional and emerging approaches to health and wellness.
5. Potential Interactions
Potential interactions constitute a critical consideration when evaluating the safety and efficacy of any plant-based alternative, especially those originating from or linked to regions and traditions historically connected to Hernn Corts. These interactions encompass the effects that botanical substances may have on other medications, supplements, or even certain foods. A lack of awareness regarding potential interactions can lead to reduced effectiveness of prescribed treatments, increased risk of adverse effects, or even life-threatening situations. The cause-and-effect relationship is straightforward: the introduction of a botanical compound alongside an existing regimen can either enhance, diminish, or alter the pharmacological activity of the other substances involved. For example, St. John’s Wort, a commonly used herbal antidepressant, is known to induce the activity of certain liver enzymes, potentially accelerating the metabolism and reducing the effectiveness of numerous medications, including oral contraceptives and immunosuppressants.
The importance of understanding potential interactions cannot be overstated. Given that many individuals seeking plant-based alternatives may already be taking prescription medications for chronic conditions, the risk of adverse interactions is significant. The integration of herbal remedies, influenced by practices from areas historically associated with Corts, must proceed with caution, involving a thorough assessment of the patient’s complete medication history and consideration of potential pharmacological incompatibilities. This necessitates open communication between patients and healthcare providers, ensuring that all relevant substances being used are disclosed and evaluated for potential interactions. Furthermore, reliable and up-to-date resources on herb-drug interactions should be consulted to inform decision-making.
In summary, a comprehensive understanding of potential interactions is an indispensable component of safe and effective plant-based therapeutics. By acknowledging the possibility of adverse interactions, clinicians and patients can collaboratively mitigate risks and optimize health outcomes. The challenge lies in promoting widespread awareness of these potential risks and fostering a culture of transparency and informed decision-making within the realm of plant-based medicine. Recognizing these interactions contributes to responsible use and safer outcomes for all parties involved and promotes the longevity of Herbal medicine.
6. Sustainability Practices
The long-term viability of “herbal alternative cortez” hinges on sustainable practices throughout the supply chain, from cultivation and harvesting to processing and distribution. Unsustainable sourcing methods can deplete natural resources, disrupt ecosystems, and threaten the availability of medicinal plants. The escalating demand for botanical remedies, coupled with irresponsible harvesting, can lead to overexploitation of wild populations, driving certain species towards endangerment or extinction. This depletion undermines the very foundation upon which these plant-based alternatives are built. The adoption of sustainable practices is therefore not merely an ethical consideration but an essential prerequisite for ensuring the continued accessibility and effectiveness of “herbal alternative cortez”.
Sustainable harvesting techniques prioritize the long-term health and regeneration of plant populations. This includes selective harvesting, allowing plants to mature and reproduce, and minimizing damage to surrounding habitats. Organic farming practices further contribute to sustainability by avoiding the use of synthetic pesticides and fertilizers, which can harm soil health and contaminate water resources. Examples of sustainable sourcing initiatives include the cultivation of medicinal plants in controlled environments, such as greenhouses and farms, and the implementation of fair trade agreements with indigenous communities, ensuring that they receive fair compensation for their knowledge and resources. These practices exemplify a commitment to environmental stewardship and social responsibility, promoting the long-term viability of “herbal alternative cortez”.
In conclusion, sustainable practices are an indispensable component of “herbal alternative cortez”. The preservation of plant biodiversity, the protection of natural resources, and the equitable treatment of indigenous communities are all integral to ensuring the continued availability and efficacy of these plant-based alternatives. By prioritizing sustainable sourcing and responsible harvesting methods, the industry can contribute to a more environmentally and socially responsible future, safeguarding the integrity and accessibility of “herbal alternative cortez” for generations to come.
Frequently Asked Questions Regarding Plant-Based Substitutes
The following addresses common inquiries concerning plant-based alternatives, providing objective and informative responses to facilitate a greater understanding of their appropriate use and limitations.
Question 1: Are plant-based substitutes invariably safer than conventional pharmaceutical medications?
Plant-based substitutes are not inherently safer than conventional pharmaceutical medications. Both categories possess the potential for adverse effects and interactions with other substances. The safety profile of any treatment, regardless of its origin, depends on factors such as dosage, individual health status, and potential interactions with other medications. Consultation with a qualified healthcare professional is essential to assess the risks and benefits of any treatment approach.
Question 2: Can plant-based substitutes completely replace conventional medical treatments for serious health conditions?
Plant-based substitutes should not be viewed as a universal replacement for conventional medical treatments, particularly in cases of serious or life-threatening health conditions. While some botanical substances may offer therapeutic benefits, they may not be sufficient to address the underlying pathology or manage acute symptoms. A comprehensive treatment plan, developed in consultation with a healthcare professional, may integrate both conventional and plant-based approaches to optimize patient outcomes.
Question 3: How can one ensure the quality and purity of plant-based products?
Ensuring the quality and purity of plant-based products requires diligence and informed decision-making. Seek products from reputable suppliers that adhere to stringent quality control standards. Look for certifications from independent organizations that verify product authenticity, purity, and potency. Examine product labels carefully to ensure accurate ingredient information and dosage instructions. Consult with a qualified herbalist or healthcare professional to identify reliable sources and verify product quality.
Question 4: What are the potential risks associated with self-treating with plant-based substitutes?
Self-treating with plant-based substitutes carries several potential risks, including misdiagnosis, improper dosage, adverse interactions with other medications, and delayed or inadequate medical care. Attempting to self-diagnose and treat medical conditions can lead to inaccurate assessments and inappropriate treatment choices, potentially worsening the underlying condition or masking symptoms. The advice of a qualified healthcare provider is essential for accurate diagnosis and treatment.
Question 5: Are there specific populations (e.g., pregnant women, children) who should avoid plant-based substitutes?
Certain populations, such as pregnant women, breastfeeding mothers, infants, and individuals with pre-existing medical conditions, require particular caution when considering plant-based substitutes. Many botanical substances have not been adequately studied for safety in these populations, and some may pose significant risks. Consultation with a qualified healthcare professional is essential to determine the appropriateness of plant-based substitutes in these cases and to identify any potential contraindications or precautions.
Question 6: Is scientific research always available to support the efficacy claims associated with plant-based substitutes?
The level of scientific evidence supporting the efficacy claims associated with plant-based substitutes varies considerably. While some botanical substances have been extensively studied and demonstrated to have therapeutic benefits, others lack robust scientific support. Traditional use and anecdotal evidence should not be considered a substitute for rigorous scientific validation. Critical evaluation of available research is essential to make informed decisions regarding the use of plant-based substitutes.
The responsible integration of plant-based substitutes into a healthcare regimen requires a balanced perspective, acknowledging both the potential benefits and the inherent risks. Informed decision-making, guided by professional expertise, is essential to optimize outcomes and minimize potential harm.
The subsequent section will delve into the legal and regulatory landscape surrounding the use of plant-based alternatives.
Conclusion
This exploration of herbal alternative cortez has illuminated critical aspects ranging from geographical origins and traditional knowledge to bioactive compounds, dosage guidelines, potential interactions, and sustainability practices. These elements collectively influence the safety, efficacy, and ethical considerations surrounding the use of plant-derived remedies. A thorough understanding of each facet is essential for responsible application and integration into healthcare strategies. The complexities inherent in botanical medicine necessitate a balanced approach, acknowledging both the potential benefits and the inherent risks associated with these alternatives.
The pursuit of knowledge regarding herbal alternative cortez should be guided by a commitment to scientific rigor, ethical sourcing, and informed decision-making. Continued research, standardized quality control, and responsible utilization are paramount to ensuring the long-term availability and safe application of plant-based remedies. Future efforts must focus on bridging the gap between traditional knowledge and modern science, fostering collaboration between researchers, healthcare professionals, and indigenous communities to unlock the full potential of botanical medicine while safeguarding its sustainability for future generations.