The term references the use of botanical remedies to manage an overactive thyroid gland. This approach involves employing various plant-derived substances with the intention of alleviating symptoms associated with excessive thyroid hormone production. For example, certain herbs are believed to possess properties that can help regulate thyroid activity or mitigate the effects of hyperthyroidism.
Throughout history, traditional medicine systems have incorporated plant-based treatments for a range of ailments, including thyroid imbalances. The perceived advantages of such remedies often include a holistic approach, focusing on overall well-being in addition to symptom management, and a potentially lower risk of severe side effects compared to conventional pharmaceutical interventions. The enduring appeal lies in the belief that nature provides gentle yet effective solutions.
The efficacy and safety of using botanical interventions for managing an overactive thyroid remain subjects of ongoing investigation. The subsequent sections will explore specific herbal options, their purported mechanisms of action, and the existing scientific evidence supporting or refuting their use, alongside critical considerations regarding potential interactions and contraindications.
The following guidelines are designed to inform individuals considering integrating plant-based remedies into their hyperthyroidism management strategy. Due diligence and professional guidance are paramount.
Tip 1: Prioritize Professional Consultation: Engaging an endocrinologist and a qualified herbalist or naturopathic doctor is crucial. A collaborative approach ensures a comprehensive understanding of both conventional and complementary treatment options, minimizing potential risks.
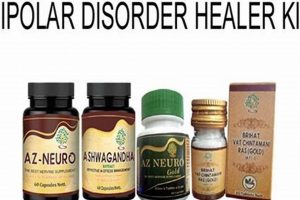
Tip 2: Verify Herbal Source and Quality: Adulteration and inconsistent potency are significant concerns in the herbal market. Selecting products from reputable manufacturers with third-party testing and verifiable sourcing practices mitigates these risks. Look for standardized extracts where available.
Tip 3: Monitor Thyroid Function Regularly: Frequent monitoring of thyroid hormone levels (TSH, T3, T4) is essential. This provides objective data on the effectiveness of any intervention and allows for timely adjustments to the treatment plan, preventing either under- or over-treatment.
Tip 4: Be Aware of Potential Interactions: Many herbs can interact with conventional medications, including thyroid hormone replacements and anti-thyroid drugs. Meticulously disclose all herbal supplements to healthcare providers to avoid adverse drug interactions.
Tip 5: Begin with Low Doses and Titrate Gradually: Starting with low doses of any new herbal supplement and gradually increasing them allows for monitoring of individual tolerance and potential side effects. This approach minimizes the risk of adverse reactions.
Tip 6: Recognize Limitations: Plant-based interventions may be more appropriate for mild cases of hyperthyroidism or as adjunctive therapy. Severe cases may require conventional medical interventions such as medication, radioiodine therapy, or surgery.
Tip 7: Research and Understand Specific Herbs: Thoroughly research the specific properties, potential benefits, and risks associated with any herb being considered for thyroid management. Reliable sources include peer-reviewed scientific literature and reputable herbal medicine databases.
Adherence to these guidelines facilitates a more informed and cautious approach, maximizing the potential benefits while minimizing risks. Individual responses to botanical remedies can vary significantly, necessitating personalized treatment plans and continuous monitoring.
This information should serve as a starting point for further exploration and discussion with qualified healthcare professionals. The following sections will provide a more in-depth examination of specific herbal options and their role in managing hyperthyroidism.
1. Botanical regulation
Botanical regulation, in the context of “hyperthyroidism herbal”, pertains to the use of plant-derived compounds to modulate thyroid gland activity. It focuses on substances believed to either inhibit thyroid hormone synthesis, reduce the conversion of T4 to T3, or otherwise influence the physiological processes contributing to excessive thyroid hormone levels.
- Inhibition of Thyroid Hormone Synthesis
Certain herbs contain compounds that may interfere with the enzymes responsible for thyroid hormone production within the thyroid gland. This can reduce the overall output of T4 and T3, potentially alleviating hyperthyroid symptoms. For example, some traditional medicines utilize plants containing substances thought to compete with iodine uptake, thereby limiting the raw materials available for hormone synthesis. However, the degree of this inhibition and its clinical significance vary depending on the specific herb and dosage.
- Reduction of T4 to T3 Conversion
The conversion of T4 (thyroxine) to T3 (triiodothyronine), the more active form of thyroid hormone, is a crucial step in thyroid hormone action. Some herbs are hypothesized to contain compounds that can inhibit the enzyme 5′-deiodinase, which is responsible for this conversion. By reducing T3 levels, these herbs may help to mitigate the effects of excessive thyroid hormone activity. Scientific evidence supporting this mechanism for specific herbs remains limited, but it is an area of ongoing research.
- Influence on Thyroid Hormone Receptors
Beyond directly affecting hormone production or conversion, some herbal constituents are proposed to influence the binding of thyroid hormones to their receptors in target tissues. This could potentially modulate the downstream effects of thyroid hormones, even if hormone levels remain elevated. This mechanism of action is less well-understood and requires further investigation to determine its clinical relevance.
- Regulation of Autoimmune Response
In cases of hyperthyroidism caused by autoimmune disorders like Graves’ disease, some herbs are believed to possess immunomodulatory properties. These herbs may help to dampen the autoimmune attack on the thyroid gland, potentially reducing thyroid hormone production. However, the effectiveness of these herbs in autoimmune hyperthyroidism is highly variable and may depend on the individual’s immune response and the severity of the condition.
The potential for botanical regulation of thyroid function highlights the complex interplay between plant-derived substances and human physiology. While traditional medicine systems have long employed herbs for thyroid imbalances, rigorous scientific investigation is essential to validate their efficacy, establish safe dosages, and understand their mechanisms of action. The use of these remedy should be approached with caution and under the guidance of qualified healthcare professionals to ensure patient safety and optimal outcomes.
2. Symptom management
Symptom management represents a critical aspect of addressing hyperthyroidism through herbal interventions. The physiological imbalances caused by excessive thyroid hormone production manifest in various symptoms, including rapid heartbeat, anxiety, weight loss, tremors, and heat intolerance. The rationale behind using plant-based remedies often lies in their potential to alleviate these discomforts, improving the patient’s quality of life even if the underlying thyroid hyperactivity is not completely resolved. The effect of herbal remedies will be various from each persons. Some botanical agents are purported to possess anxiolytic properties, potentially mitigating anxiety and nervousness associated with hyperthyroidism. Others may have mild sedative effects, aiding in sleep and reducing restlessness. Furthermore, certain herbs have traditionally been used to address cardiovascular symptoms such as palpitations. The impact of these treatments on the root cause of the disease needs comprehensive treatments.
The practical significance of symptom management in hyperthyroidism lies in its ability to bridge the gap between diagnosis and definitive treatment, or to complement conventional medical interventions. While waiting for diagnostic tests or initiating pharmaceutical therapy, or during periods when medication adjustments are being made, plant-based remedies may offer a degree of symptomatic relief. For instance, an individual experiencing mild to moderate anxiety and insomnia due to hyperthyroidism might find temporary benefit from herbs traditionally used for relaxation and sleep promotion. Such relief can be valuable in maintaining daily functioning and overall well-being. Also, some evidence showed herbal remedy for thyroid disease.
Effective symptom management using herbal approaches requires a cautious and individualized strategy. Not all herbs are safe or effective for all individuals, and potential interactions with conventional medications must be carefully considered. It is crucial to consult with a qualified healthcare professional, including both an endocrinologist and a knowledgeable herbalist or naturopathic doctor, to develop a safe and appropriate treatment plan. A holistic understanding of the patient’s health status, symptom presentation, and potential risks is essential to optimize the benefits of herbal interventions while minimizing potential adverse effects. As a result, the management will not be suitable for all cases, or as an alternative treatment.
3. Traditional usage
Traditional usage forms a foundational element within the concept of “hyperthyroidism herbal,” representing the accumulated knowledge and practices passed down through generations concerning the application of plant-based remedies for thyroid imbalances. This historical context provides a starting point for understanding which botanicals have been empirically observed to influence thyroid function or alleviate related symptoms. The cause-and-effect relationships, as understood within these traditional systems, often stem from direct observation of patient responses to specific herbal preparations. For instance, in some traditional medicine systems, certain plants were administered to individuals exhibiting symptoms suggestive of hyperthyroidism, such as rapid heartbeat, anxiety, and weight loss. The observed reduction in these symptoms following herbal administration led to the association of those plants with thyroid-related conditions.
The importance of traditional usage lies in its potential to guide modern research and drug discovery. While traditional practices may lack the rigorous scientific methodology of contemporary medicine, they offer a rich source of information regarding potentially bioactive compounds and their therapeutic applications. For example, traditional herbal texts may describe the use of specific plants to “cool” the body, thereby alleviating heat intolerance, a common symptom of hyperthyroidism. Modern researchers can then investigate the phytochemical composition of these plants to identify the compounds responsible for this effect and assess their efficacy and safety through clinical trials. However, it is crucial to acknowledge the limitations of traditional knowledge. The absence of standardized dosages, variations in herbal preparations, and the lack of controlled studies make it difficult to directly translate traditional practices into modern medical applications.
Understanding the traditional usage of herbal remedies for hyperthyroidism offers a valuable perspective, serving as a bridge between historical practices and evidence-based medicine. While not a substitute for conventional medical care, it can inform research, guide the selection of potentially beneficial herbs, and promote a more holistic approach to managing thyroid imbalances. The integration of traditional knowledge with modern scientific methods holds the potential to uncover novel therapeutic strategies, provided that safety and efficacy are rigorously evaluated. The challenge lies in discerning valid observations from anecdotal evidence and applying scientific rigor to validate the potential benefits of traditionally used herbs.
4. Scientific validation
Scientific validation, in the context of “hyperthyroidism herbal,” refers to the application of rigorous scientific methodologies to assess the efficacy and safety of plant-derived remedies for managing overactive thyroid conditions. This process is essential for determining whether traditional uses and anecdotal evidence are supported by quantifiable data and for identifying potential risks associated with herbal interventions.
- Controlled Clinical Trials
Randomized, placebo-controlled clinical trials represent the gold standard for evaluating the effectiveness of herbal treatments. These studies involve comparing the effects of a specific herb or herbal formulation to a placebo or standard medication in individuals with hyperthyroidism. Key outcome measures include changes in thyroid hormone levels (TSH, T3, T4), symptom severity scores, and quality of life assessments. Positive results from well-designed clinical trials provide strong evidence supporting the use of a particular herb for hyperthyroidism management. For example, a clinical trial evaluating the impact of Lycopus virginicus (bugleweed) on thyroid hormone levels could provide data on its potential to inhibit thyroid hormone synthesis.
- Phytochemical Analysis and Mechanism of Action Studies
Identifying the active compounds within an herb and elucidating their mechanisms of action is crucial for understanding how it might affect thyroid function. Phytochemical analysis involves isolating and characterizing the chemical constituents of an herb, while mechanism of action studies investigate how these compounds interact with the body’s biological systems. This research can reveal whether an herb directly inhibits thyroid hormone production, modulates the immune system, or influences other relevant pathways. For example, identifying the specific compounds in Melissa officinalis (lemon balm) that contribute to its purported anti-thyroid effects, and determining how these compounds interact with thyroid hormone receptors, would provide valuable insights.
- Safety and Toxicity Assessments
Assessing the safety and potential toxicity of herbal remedies is paramount. This involves conducting preclinical studies (e.g., in vitro and animal studies) to evaluate the herb’s effects on various organ systems and to identify potential adverse effects. Clinical trials also play a crucial role in monitoring for side effects and drug interactions. Rigorous safety assessments are essential for determining the appropriate dosage and identifying contraindications. For example, investigating the potential hepatotoxicity or nephrotoxicity of long-term use of certain herbal formulations would be a critical aspect of scientific validation.
- Standardization and Quality Control
Ensuring the consistency and quality of herbal products is essential for reliable scientific validation. Standardization involves establishing specific quality control measures to guarantee that each batch of an herbal product contains a consistent amount of active compounds. This is important because the concentration of active compounds can vary significantly depending on factors such as plant species, growing conditions, and extraction methods. Quality control measures help to ensure that herbal products are free from contaminants and adulterants. Reliable validation can be done by doing such actions as chromatography and spectometry.
These facets collectively underscore the importance of scientific validation in assessing the utility of “hyperthyroidism herbal.” The application of rigorous research methodologies, including controlled clinical trials, phytochemical analysis, safety assessments, and standardization efforts, is essential for determining whether plant-derived remedies offer genuine benefits for managing overactive thyroid conditions. Without scientific validation, the use of herbal interventions remains speculative and potentially risky. Thus, healthcare professionals and patients should prioritize evidence-based approaches when considering herbal options for hyperthyroidism management.
5. Potential interactions
The use of plant-based remedies for hyperthyroidism demands careful consideration of potential interactions with conventional medications and other substances. Due to the complex biochemical profiles of herbs, interactions can occur through various mechanisms, influencing the absorption, metabolism, or excretion of both herbal components and pharmaceutical drugs. This is especially critical given that hyperthyroidism often requires concurrent treatment with anti-thyroid medications such as methimazole or propylthiouracil. For example, an herb might potentiate the effects of an anti-thyroid drug, leading to hypothyroidism, or conversely, diminish its efficacy, exacerbating hyperthyroid symptoms.
Examples of clinically relevant interactions include the effects of iodine-containing herbs. While iodine is essential for thyroid hormone synthesis, excessive iodine intake can paradoxically worsen hyperthyroidism in certain individuals, particularly those with autonomous thyroid nodules or iodine-induced hyperthyroidism. Similarly, some herbs possess anticoagulant properties, which could increase the risk of bleeding when combined with anti-thyroid medications that can also affect blood clotting. Another concern is the potential for herbs to affect liver enzymes responsible for drug metabolism. This could alter the levels of anti-thyroid drugs in the body, leading to either toxicity or therapeutic failure. Furthermore, certain dietary supplements, such as those containing high doses of vitamin D or calcium, may interfere with the absorption of thyroid hormone replacement medication if hypothyroidism develops as a consequence of anti-thyroid treatment or herbal interventions.
Understanding potential interactions is paramount for safe and effective hyperthyroidism management. A comprehensive assessment of a patient’s medication and supplement history, coupled with knowledge of herbal pharmacology, is essential to minimize risks. Healthcare providers should advise patients to disclose all herbal and dietary supplements they are using, and to closely monitor thyroid hormone levels and clinical symptoms during concurrent use of herbs and conventional medications. Given the potential for adverse effects, herbal remedies for hyperthyroidism should be employed cautiously, under the guidance of qualified healthcare professionals, and with consideration of evidence-based guidelines.
6. Holistic approach
The holistic approach, when applied to hyperthyroidism herbal interventions, emphasizes treating the individual as a whole, considering the interconnectedness of physical, mental, and emotional well-being, rather than focusing solely on thyroid hormone levels. This perspective acknowledges that hyperthyroidism symptoms often extend beyond physiological imbalances and can significantly impact a person’s overall quality of life.
- Stress Management Integration
Hyperthyroidism frequently exacerbates anxiety and stress. A holistic approach incorporates stress-reduction techniques such as mindfulness meditation, yoga, or deep breathing exercises to mitigate these symptoms. By addressing the psychological impact of hyperthyroidism, the patient’s overall response to herbal remedies may be enhanced, leading to more effective symptom management. Example: A patient experiencing insomnia and anxiety due to hyperthyroidism may benefit from chamomile tea alongside herbal treatments targeting thyroid function, promoting relaxation and improved sleep.
- Dietary and Nutritional Considerations
A holistic approach emphasizes the importance of a balanced diet rich in nutrients that support thyroid health and overall well-being. This may involve avoiding processed foods, reducing caffeine intake, and incorporating foods rich in antioxidants and essential minerals. A registered dietitian can help create a personalized nutrition plan that complements herbal treatments. Example: A patient with hyperthyroidism may benefit from reducing their intake of iodine-rich foods while incorporating foods that support adrenal function, as adrenal fatigue can be a contributing factor to the condition.
- Lifestyle Modifications and Exercise
Regular physical activity, tailored to the individual’s tolerance and physical limitations, is a key component of a holistic approach. Exercise can help manage weight, improve mood, and reduce stress levels. However, it is crucial to avoid overexertion, as this can exacerbate hyperthyroid symptoms. Gentle forms of exercise, such as walking or swimming, may be more appropriate. Example: A patient with hyperthyroidism might benefit from a structured exercise program that includes low-impact activities and focuses on building strength and endurance gradually, while monitoring their heart rate and energy levels.
- Addressing Underlying Emotional Factors
Some practitioners believe that unresolved emotional issues can contribute to thyroid imbalances. A holistic approach may involve exploring these underlying factors through counseling or therapy. Addressing emotional stressors can potentially reduce the body’s overall stress response and support thyroid function. Example: A patient with hyperthyroidism who identifies significant emotional stressors through therapy may experience a reduction in anxiety and other hyperthyroid symptoms, potentially enhancing the effectiveness of herbal interventions.
These facets illustrate how a holistic approach integrates various lifestyle and emotional considerations alongside the use of “hyperthyroidism herbal” treatments. The emphasis on treating the individual as a whole, rather than solely focusing on thyroid hormone levels, reflects a broader perspective on health and well-being, potentially leading to more effective and sustainable outcomes. It is crucial to emphasize, however, that such an approach requires close collaboration with qualified healthcare professionals, including endocrinologists, herbalists, and mental health specialists, to ensure safety and efficacy.
Frequently Asked Questions
The following section addresses common inquiries regarding the use of plant-based remedies for managing hyperthyroidism, providing evidence-based information to inform decision-making.
Question 1: Are herbal remedies a safe and effective alternative to conventional hyperthyroidism treatments?
Herbal remedies should not be considered a direct replacement for conventional medical treatments such as anti-thyroid medications, radioiodine therapy, or surgery. While some herbs may offer symptomatic relief or play a supportive role, their efficacy in directly controlling thyroid hormone production is often limited. Consulting with an endocrinologist is crucial for determining the most appropriate treatment approach, particularly in cases of moderate to severe hyperthyroidism.
Question 2: Which herbs are commonly used in hyperthyroidism herbal approaches?
Several herbs are traditionally associated with thyroid support, including Lycopus virginicus (bugleweed), Melissa officinalis (lemon balm), and Leonurus cardiaca (motherwort). These herbs are believed to possess properties that may inhibit thyroid hormone synthesis, reduce anxiety, or alleviate palpitations. However, scientific evidence supporting their efficacy varies, and more rigorous research is needed to confirm their benefits.
Question 3: What are the potential risks associated with herbal remedies for hyperthyroidism?
Herbal remedies can pose several risks, including allergic reactions, drug interactions, and inconsistent product quality. Some herbs may interact with conventional medications, altering their effectiveness or increasing the risk of side effects. It is crucial to inform healthcare providers about all herbal supplements being taken to avoid potential complications. Selecting products from reputable manufacturers with third-party testing can help mitigate the risk of contamination and adulteration.
Question 4: How can one ensure the quality and safety of herbal products?
Selecting herbal products from reputable manufacturers that adhere to Good Manufacturing Practices (GMP) is essential. Look for products that have undergone third-party testing for purity, potency, and contaminants. Standardized extracts, which contain a consistent amount of active compounds, are often preferred. Consulting with a qualified herbalist or naturopathic doctor can provide guidance on selecting appropriate products and dosages.
Question 5: Can herbal remedies completely cure hyperthyroidism?
There is currently no scientific evidence to support the claim that herbal remedies can completely cure hyperthyroidism. While some herbs may offer symptomatic relief or play a supportive role in managing the condition, they do not address the underlying causes of thyroid hyperactivity in many cases. Conventional medical treatments, such as anti-thyroid medications or radioiodine therapy, are often necessary to achieve long-term control of thyroid hormone levels.
Question 6: How does one integrate herbal remedies into a conventional hyperthyroidism treatment plan safely?
The integration of herbal remedies into a conventional hyperthyroidism treatment plan should be done cautiously and under the guidance of qualified healthcare professionals. It is crucial to consult with both an endocrinologist and a knowledgeable herbalist or naturopathic doctor to develop a safe and appropriate treatment strategy. Regular monitoring of thyroid hormone levels and clinical symptoms is essential to assess the effectiveness of herbal interventions and to make necessary adjustments to the treatment plan.
The judicious use of herbal remedies may offer supportive benefits in managing hyperthyroidism, however should not replace standard medical treatment.
The subsequent section presents concluding remarks and provides further resources for informed decision-making.
Conclusion
This exploration of “hyperthyroidism herbal” has presented a spectrum of considerations, spanning traditional applications to contemporary scientific inquiry. While botanical remedies hold historical significance and potential for symptom management, their role in directly addressing hyperthyroidism requires careful scrutiny. The interplay between herbal constituents and thyroid physiology is complex, necessitating rigorous research to validate efficacy and ensure patient safety. The information here highlights an important area of traditional application but does not serve as a replacement to professional medical advice or treatments.
Given the potential for interactions and the limitations of current scientific evidence, a cautious and informed approach is paramount. Prioritizing professional medical guidance, coupled with thorough research and responsible product selection, remains essential for those considering incorporating plant-based interventions into their hyperthyroidism management strategy. The ongoing exploration of botanical medicine offers promise, but responsible integration requires a commitment to evidence-based decision-making. Any treatment for hyperthyroidism should be consulted with healthcare professionals.