The concept refers to the utilization of plants and their extracts to potentially influence systemic arterial pressure. This approach encompasses a wide range of botanical substances, prepared in various forms such as teas, capsules, or tinctures, aimed at contributing to the maintenance of healthy circulatory function.
Throughout history, numerous cultures have incorporated botanical remedies into traditional medical practices for cardiovascular wellness. Proponents suggest that certain plants possess properties that may support healthy blood vessel function, contribute to normal fluid balance, and promote overall cardiovascular health. However, the efficacy and safety of these remedies require thorough scientific evaluation.
The subsequent sections will explore specific botanicals commonly associated with supporting healthy circulatory function, examine the existing scientific evidence regarding their effectiveness, and discuss crucial considerations related to their safe and responsible use.
Considerations for Botanical Approaches to Systemic Arterial Pressure
The following considerations are offered for individuals exploring botanical interventions to support healthy systemic arterial pressure. It is crucial to approach these options with informed awareness and professional guidance.
Tip 1: Consult a Qualified Healthcare Professional: Prior to initiating any botanical regimen, a thorough consultation with a physician, ideally one with expertise in integrative medicine, is imperative. This consultation should include a comprehensive review of medical history, current medications, and potential interactions.
Tip 2: Prioritize Evidence-Based Options: While anecdotal evidence abounds, emphasis should be placed on botanicals with demonstrable efficacy supported by rigorous clinical trials. Research peer-reviewed studies to assess the level of evidence backing a particular plant or extract.
Tip 3: Adhere to Recommended Dosages: Botanical substances are not inherently benign. Precise adherence to recommended dosages, typically established through clinical research or under the guidance of a healthcare professional, is vital to minimize potential adverse effects.
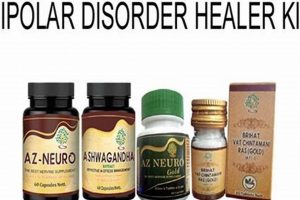
Tip 4: Source Products from Reputable Suppliers: The quality and purity of botanical products can vary substantially. Opt for suppliers with third-party certifications verifying product content, potency, and absence of contaminants such as heavy metals or pesticides.
Tip 5: Monitor Systemic Arterial Pressure Regularly: Self-monitoring of systemic arterial pressure, using a validated device and following established protocols, is essential to assess the impact of botanical interventions and to detect any concerning changes.
Tip 6: Be Vigilant for Adverse Reactions: Discontinue use immediately and seek medical attention if any adverse reactions, such as allergic symptoms, gastrointestinal distress, or changes in heart rate, occur.
Tip 7: Understand Potential Interactions: Many botanical substances can interact with conventional medications, potentially altering their efficacy or increasing the risk of side effects. A thorough review of potential interactions with a pharmacist or physician is crucial.
Adherence to these considerations promotes a safe and informed approach to the utilization of botanicals for supporting healthy systemic arterial pressure. The information is intended to augment, not replace, the advice of qualified healthcare providers.
The following section will discuss potential risks and considerations to support informed decision-making.
1. Botanical Identification
Accurate botanical identification forms the bedrock of any responsible application of plants aimed at supporting healthy systemic arterial pressure. The substitution of one plant species for another, even within the same genus, can lead to markedly different, and potentially adverse, physiological effects. The chemical composition of plants varies considerably based on species, subspecies, and even environmental factors, resulting in differing concentrations of active compounds. This variability directly influences the intended therapeutic outcome and the risk profile associated with its use.
A practical example highlighting the importance of precise identification can be found in the use of hawthorn. While Crataegus monogyna and Crataegus laevigata are both commonly referred to as hawthorn and possess cardiovascular properties, their specific chemical profiles differ, potentially affecting their efficacy and safety profiles. In cases where standardized extracts are utilized, the specific species from which the extract is derived must be clearly identified and verified through appropriate analytical techniques, such as High-Performance Liquid Chromatography (HPLC), to ensure consistency and predictability of effect. Failure to accurately identify the plant can lead to ineffective treatment or, worse, adverse health consequences due to unintended interactions or toxicity.
In summary, botanical identification is not merely a taxonomic exercise, but a critical safety measure when considering the use of plants. It minimizes risk, promotes consistent outcomes, and enables responsible integration of plant-based approaches into a holistic health strategy. The challenges involved in ensuring accurate botanical identification underscore the need for expert consultation and procurement of products from reputable sources that prioritize quality control. It is crucial for overall patient safety and efficacy, and it is paramount to maintain best practices.
2. Preparation Methods
The method by which a botanical substance is prepared significantly impacts its bioavailability and, consequently, its potential effect on systemic arterial pressure. Different extraction techniques yield varying concentrations of active compounds, thereby influencing the overall potency and therapeutic efficacy of the preparation. For instance, an aqueous extract (tea) of a plant may contain a different spectrum and concentration of bioactive constituents compared to an alcoholic tincture or a supercritical fluid extract. The choice of preparation method, therefore, represents a critical determinant of the ultimate physiological effect.
Consider the preparation of hawthorn ( Crataegus spp.), often utilized to support healthy circulatory function. A simple hot water infusion (tea) may extract readily soluble compounds but may not efficiently extract more complex or fat-soluble constituents. Conversely, a prolonged maceration in alcohol will likely extract a broader range of compounds, potentially including those with greater influence on blood vessel relaxation. Furthermore, factors such as particle size, temperature, and duration of extraction all contribute to the final composition of the prepared botanical remedy, and the method should be evidence-based and standardized to ensure the stability and reproducibility of the desired benefit.
In conclusion, understanding the connection between preparation methods and their effect on the resulting botanical composition is indispensable for achieving consistent and predictable outcomes. The selection of an appropriate preparation method is a critical decision that influences the concentration and availability of active compounds and impacts the efficacy of herbal remedies for blood pressure support. This knowledge is fundamental for healthcare practitioners and informed consumers alike, necessitating careful consideration of the specific botanical, its intended use, and the properties of the selected preparation method.
3. Dosage Standardization
Dosage standardization constitutes a pivotal element in the responsible and effective utilization of botanicals intended to influence systemic arterial pressure. The inherent variability in plant composition necessitates meticulous attention to dosage to ensure consistent therapeutic outcomes and minimize the potential for adverse effects.
- Variability in Plant Composition
Botanical substances are derived from natural sources, and their chemical makeup can vary significantly based on factors such as geographical location, growing conditions, harvesting practices, and storage methods. This variability directly affects the concentration of active compounds present in the final product, making precise dosage essential for consistent effects.
- Impact on Therapeutic Efficacy
A standardized dosage aims to deliver a predictable quantity of the key bioactive constituents believed to be responsible for the desired physiological effects. Without standardization, the therapeutic effect of a botanical remedy can be unpredictable, ranging from inefficacy to potentially harmful overexposure. For instance, a hawthorn extract intended to support healthy circulatory function requires a standardized level of specific flavonoids to achieve the intended effects.
- Minimizing Adverse Effects
Proper dosage standardization is crucial in mitigating the risk of adverse effects associated with botanical remedies. Overconsumption of certain plant compounds can lead to toxic reactions or interactions with conventional medications. Standardized dosages, based on scientific research and established safety profiles, help ensure that individuals receive a safe and effective amount of the botanical substance.
- Role of Extraction Techniques
The extraction technique used to derive the botanical substance significantly influences the final composition and concentration of active compounds. Standardization requires not only specifying the dosage but also the extraction method employed, ensuring consistency in the extraction process to obtain predictable therapeutic outcomes. For example, extracting ginkgo leaves using different solvents can yield variations in the concentration of ginkgolides and bilobalide, necessitating different dosage adjustments.
The discussed facets highlight the importance of dosage standardization. Neglecting this critical aspect can undermine the potential benefits of plants while increasing the risks. This ensures a consistent delivery of active compounds, ultimately promoting safe and effective management of healthy systemic arterial pressure using botanical interventions.
4. Potential Interactions
The confluence of botanical substances and conventional pharmaceuticals within a single treatment regimen necessitates careful consideration of potential interactions. These interactions can manifest in various ways, altering the absorption, distribution, metabolism, or excretion (ADME) of either the botanical or the drug, leading to altered efficacy or heightened toxicity. The impact on systemic arterial pressure can be either synergistic, leading to excessive reductions, or antagonistic, negating the intended effects of antihypertensive medications. This is not an inconsequential theoretical risk, but a clinically relevant concern.
For instance, the concurrent use of garlic ( Allium sativum ), which possesses mild blood-thinning properties, with anticoagulant medications such as warfarin can potentiate the anticoagulant effect, increasing the risk of bleeding. Similarly, certain herbal diuretics, when combined with prescription diuretics, can lead to excessive potassium depletion, resulting in electrolyte imbalances and potentially serious cardiovascular complications. Furthermore, botanicals known to affect liver enzyme activity, such as St. John’s Wort ( Hypericum perforatum), can significantly alter the metabolism of various antihypertensive drugs, either reducing their effectiveness or increasing their concentration to toxic levels.
Therefore, a comprehensive evaluation of potential interactions is paramount before incorporating any botanical substance into a treatment plan aimed at managing systemic arterial pressure. This evaluation should involve a thorough review of the patient’s medication list, including both prescription and over-the-counter drugs, as well as a detailed understanding of the pharmacological properties of the botanical in question. Collaboration between healthcare providers, including physicians, pharmacists, and qualified herbalists, is essential to mitigate the risk of adverse interactions and ensure patient safety.
5. Efficacy Validation
Efficacy validation, in the context of herbal substances aimed at influencing systemic arterial pressure, constitutes a critical scientific process. It is the cornerstone upon which the responsible utilization of botanicals for cardiovascular support rests, determining whether the claims associated with these substances are substantiated by rigorous evidence.
- Randomized Controlled Trials (RCTs)
RCTs are the gold standard for efficacy validation. These trials involve randomly assigning participants to either a treatment group receiving the herbal substance or a control group receiving a placebo. By comparing outcomes between these groups, researchers can determine whether the botanical has a statistically significant effect on systemic arterial pressure. Example: a double-blind RCT examining the impact of hawthorn extract on individuals with mild hypertension provides a high level of evidence regarding its potential to lower blood pressure.
- Meta-Analyses and Systematic Reviews
These analyses synthesize the results of multiple independent studies on a specific herbal substance. By pooling data from various trials, meta-analyses can provide a more comprehensive assessment of efficacy and identify potential sources of heterogeneity. Systematic reviews involve a rigorous and transparent methodology to identify, evaluate, and summarize the available evidence. For example, a systematic review of studies investigating the effect of hibiscus tea on blood pressure can provide an overview of the evidence base and highlight any limitations or inconsistencies.
- Dosage and Formulation Considerations
Efficacy validation must encompass careful consideration of dosage and formulation. The effectiveness of a botanical substance can vary significantly depending on the dosage used, the method of preparation, and the presence of other ingredients. Studies should clearly define the specific dosage and formulation used to allow for replication and comparison across trials. For example, an extract of garlic might require a specific allicin content to achieve the blood pressure-lowering effects observed in clinical trials.
- Long-Term Effects and Safety
Efficacy validation should not only assess the immediate impact of a botanical substance on systemic arterial pressure but also evaluate its long-term effects and safety profile. Long-term studies are necessary to determine whether the benefits of the botanical are sustained over time and to identify any potential adverse effects that may emerge with prolonged use. Example: A long-term observational study following individuals who regularly consume beetroot juice, assessing both blood pressure control and any associated health risks.
These facets of efficacy validation underscore the critical importance of rigorous scientific investigation to determine the true potential and limitations of botanicals for blood pressure management. Claims regarding the efficacy of “herbal blood pressure” remedies must be substantiated by robust evidence to ensure responsible and safe utilization.
6. Safety Monitoring
The integration of rigorous safety monitoring protocols is paramount when employing botanicals to influence systemic arterial pressure. Due to the inherent biological activity of herbal substances, and the potential for interactions with conventional pharmaceuticals, vigilance in tracking physiological responses and adverse events is non-negotiable. The absence of robust monitoring can lead to delayed detection of adverse reactions, masking of underlying health issues, and an underestimation of the true risk associated with botanical interventions. A proactive safety monitoring strategy is essential to protect patient well-being and ensure that the purported benefits of botanicals outweigh potential harm.
Examples of necessary safety monitoring include regular self-monitoring of systemic arterial pressure. In addition, monitoring for symptoms of hypotension (dizziness, lightheadedness) or interactions with other medications is crucial. Regular blood tests may be required to assess kidney and liver function to ensure that the botanical substances are not causing any organ damage. Specific populations, such as pregnant women or individuals with pre-existing medical conditions, warrant even closer supervision due to increased susceptibility to adverse effects. Lack of careful monitoring can result in severe consequences.
In conclusion, safety monitoring is not an ancillary aspect of utilizing plants. It is an indispensable component. Implementing comprehensive monitoring strategies, driven by evidence-based guidelines, is essential to ensure the safe and effective integration of botanical substances into an approach aimed at supporting healthy systemic arterial pressure. Failing to prioritize this aspect compromises the well-being of individuals, reduces the credibility of botanical interventions, and hinders advancements in our understanding of their potential benefits and risks.
Frequently Asked Questions about Botanical Approaches
The following addresses common inquiries surrounding the usage of plants for potential support of systemic arterial pressure. These answers are intended for informational purposes and do not substitute professional medical advice.
Question 1: Are botanical substances a safe alternative to conventional hypertension medications?
Botanical substances are not inherently safe alternatives. The safety and efficacy depend on factors such as the specific plant, dosage, individual health status, and potential interactions with medications. Consultation with a qualified healthcare professional is essential before considering botanical options.
Question 2: Can botanicals completely replace prescription medications for hypertension?
Botanicals should not be used as a replacement for prescribed antihypertensive medications without the explicit guidance and supervision of a qualified healthcare provider. Discontinuing prescribed medication without medical supervision can lead to serious health risks.
Question 3: How are botanical dosages determined for blood pressure support?
Botanical dosages are determined through scientific research and traditional knowledge. However, the optimal dosage can vary based on individual factors and the specific formulation. Adherence to recommended dosages and consultation with a healthcare professional are crucial.
Question 4: Are there potential side effects associated with botanical substances for blood pressure?
Botanical substances can have side effects, including allergic reactions, gastrointestinal upset, and interactions with medications. It is imperative to be aware of potential side effects and to discontinue use if any adverse reactions occur.
Question 5: How can one ensure the quality and purity of botanical products for blood pressure support?
Ensuring quality and purity requires sourcing products from reputable suppliers with third-party certifications. These certifications verify product content, potency, and the absence of contaminants. Thorough research and scrutiny of product labels are essential.
Question 6: Can botanicals be used safely in conjunction with conventional hypertension medications?
Combining botanicals with conventional medications carries a risk of interactions that can either enhance or diminish the effects of either substance. A comprehensive review with a healthcare provider, including a pharmacist, is crucial to assess and mitigate potential interactions.
In summary, the information provided is not exhaustive and does not constitute medical advice. It is intended to promote informed decision-making in consultation with qualified healthcare professionals.
This completes the discussion of frequently asked questions. The following section will provide resources for further learning.
Concluding Remarks on Herbal Blood Pressure
This exploration has underscored the complexities inherent in utilizing botanical substances to potentially influence systemic arterial pressure. The efficacy validation, dosage standardization, and safety monitoring aspects presented highlight the necessity for rigorous scientific evaluation and responsible application. The potential for interactions with conventional pharmaceuticals further emphasizes the importance of careful consideration and professional guidance.
Moving forward, a continued emphasis on evidence-based research, stringent quality control measures, and collaborative healthcare approaches is paramount. The responsible and informed use of botanical interventions requires a commitment to patient safety and a cautious approach to unsubstantiated claims. Additional research would further support effective and safe practice.