The use of botanical remedies to alleviate the symptoms of a chronic autoimmune disease characterized by inflammation of the joints, resulting in pain, swelling, stiffness, and loss of function, represents a significant area of interest for individuals seeking alternative or complementary treatment options. This approach involves employing various plant-derived substances, often prepared as teas, tinctures, capsules, or topical applications, with the intention of reducing inflammation, managing pain, and improving overall joint health.
The potential advantage lies in the utilization of substances with purportedly fewer side effects compared to conventional pharmaceuticals, while also appealing to a preference for natural interventions. Historically, many cultures have relied on traditional medicine, including plant-based therapies, for managing a wide range of ailments, including inflammatory conditions. The appeal of this approach is further enhanced by the desire for a more holistic and personalized approach to healthcare, emphasizing the body’s innate healing capabilities.
The subsequent discussion will explore specific botanicals that have been investigated for their potential therapeutic effects on this particular autoimmune condition. Attention will be given to the scientific evidence supporting their use, potential mechanisms of action, safety considerations, and the importance of consulting with qualified healthcare professionals before incorporating any herbal remedies into a treatment plan. The examination will provide a comprehensive overview of the role of phytotherapy in the context of managing this challenging and debilitating disease.
Guidance on Botanical Remedies for Rheumatoid Arthritis
The following guidelines offer essential considerations for individuals exploring plant-based approaches to manage rheumatoid arthritis symptoms. These recommendations emphasize informed decision-making and responsible integration with conventional medical care.
Tip 1: Research Thoroughly: Investigate credible scientific evidence regarding the efficacy and safety of any botanical remedy considered. Peer-reviewed studies and reputable herbal medicine resources are essential for informed evaluation.
Tip 2: Consult a Healthcare Professional: Seek advice from a qualified physician or rheumatologist before initiating any plant-based treatment. This ensures compatibility with existing medications and appropriate monitoring of disease activity.
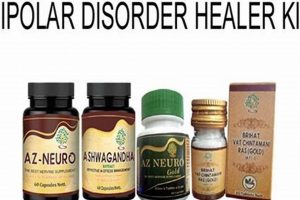
Tip 3: Identify Reputable Sources: Procure herbal products from established and trustworthy suppliers adhering to Good Manufacturing Practices (GMP). This minimizes the risk of contamination, adulteration, or misidentification of plant species.
Tip 4: Understand Potential Interactions: Be aware that certain botanicals may interact with conventional pharmaceuticals, potentially altering their effectiveness or increasing the risk of adverse effects. Full disclosure of all supplements used is crucial for healthcare providers.
Tip 5: Monitor for Adverse Reactions: Closely observe for any unexpected or undesirable symptoms following the introduction of a botanical remedy. Discontinue use immediately and seek medical attention if adverse reactions occur.
Tip 6: Manage Expectations: Understand that plant-based therapies may offer symptomatic relief but are unlikely to provide a complete cure for rheumatoid arthritis. Realistic goals are essential for successful integration into a comprehensive treatment plan.
Tip 7: Consider Formulations and Dosage: Different preparations and dosages can significantly affect the action of herbal remedies. Follow recommended dosage guidelines closely and understand the differences between extracts, tinctures, and whole herb preparations.
Tip 8: Focus on Holistic Health: Complement herbal remedies with lifestyle modifications known to benefit rheumatoid arthritis, such as a balanced diet, regular exercise, stress management techniques, and adequate rest.
These tips emphasize the importance of responsible and informed integration of plant-based remedies for rheumatoid arthritis, reinforcing that safety and evidence-based decision-making are paramount.
Adhering to these guidelines can facilitate a more comprehensive and safer approach to managing rheumatoid arthritis symptoms, warranting collaborative effort between individuals and their healthcare providers.
1. Anti-inflammatory potential
The purported connection between botanical agents and rheumatoid arthritis management frequently hinges on the anti-inflammatory properties attributed to various plant compounds. Rheumatoid arthritis, an autoimmune disorder characterized by chronic inflammation of the joints, presents a therapeutic target for agents capable of modulating inflammatory pathways. The premise is that substances with inherent anti-inflammatory capabilities may mitigate the disease’s progression and alleviate associated symptoms such as pain, swelling, and stiffness. For instance, compounds like curcumin found in turmeric, and boswellic acids derived from Boswellia serrata, have demonstrated anti-inflammatory effects in laboratory and preclinical studies. These effects are often attributed to their ability to inhibit inflammatory mediators, such as cytokines and enzymes involved in the inflammatory cascade.
However, the translation of observed anti-inflammatory potential in vitro or in animal models to demonstrable clinical efficacy in human subjects with rheumatoid arthritis requires careful consideration. While some clinical trials have suggested potential benefits of specific botanical extracts in reducing pain and inflammation scores, methodological limitations, small sample sizes, and variations in product standardization often complicate the interpretation of results. Furthermore, the bioavailability of certain compounds, such as curcumin, can be limited, necessitating specialized formulations to enhance absorption and utilization. Therefore, relying solely on the inherent anti-inflammatory potential of an herbal remedy without rigorous clinical validation presents a potential risk of overestimation of its therapeutic benefit.
In summary, the anti-inflammatory potential of certain botanicals offers a rationale for their exploration as adjunctive treatments for rheumatoid arthritis. However, the available scientific evidence necessitates caution. The observed anti-inflammatory activity in laboratory settings does not automatically translate to significant clinical improvement. Responsible application requires a comprehensive understanding of the limitations of existing research, the potential for individual variability in response, and the importance of integrating plant-based therapies within a framework of conventional medical care and oversight.
2. Symptom management strategies
Strategies aimed at managing the symptoms of rheumatoid arthritis often encompass a multifaceted approach, incorporating both conventional pharmaceutical interventions and complementary therapies. The utilization of plant-derived substances forms a subset of these complementary strategies, with the purported goal of alleviating specific manifestations of the disease. Effective symptom management necessitates a clear understanding of the interplay between the underlying pathology of rheumatoid arthritis and the mechanisms of action associated with particular botanicals. For example, ginger extracts, known for their potential anti-inflammatory properties, may be employed to reduce joint pain and stiffness. Willow bark, containing salicin, a precursor to aspirin, has been historically utilized as an analgesic for pain relief. The practical significance lies in the potential to reduce reliance on conventional pain medications or to provide an additional avenue for symptom control when conventional treatments prove insufficient.
The selection of appropriate botanical agents for symptom management should be guided by evidence-based principles whenever possible. Clinical trials, albeit often limited in scope and methodological rigor, provide insights into the efficacy and safety of specific herbal preparations. Furthermore, individual factors, such as the severity and specific nature of symptoms, concurrent medications, and potential allergies, should be carefully considered. A personalized approach, involving consultation with a qualified healthcare professional, is paramount to ensure that the chosen herbal remedies are appropriate and do not pose any undue risks. The lack of standardization in herbal products represents a challenge. Variations in plant species, harvesting practices, and extraction methods can influence the potency and composition of these substances, leading to inconsistencies in therapeutic effects.
In summary, symptom management strategies utilizing plant-derived substances offer a potential avenue for alleviating the discomfort associated with rheumatoid arthritis. However, this approach should not be viewed as a replacement for conventional medical care. Rather, it should be integrated into a comprehensive treatment plan under the guidance of a qualified healthcare professional. The challenges associated with standardization, limited evidence, and potential interactions necessitate a cautious and informed approach, emphasizing patient safety and realistic expectations.
3. Scientific validation gaps
The concept of a definitive plant-derived treatment for rheumatoid arthritis is significantly undermined by substantial deficiencies in scientific validation. Rigorous clinical trials, the cornerstone of evidence-based medicine, are frequently lacking for many botanical remedies touted for their potential therapeutic effects. This absence creates a critical knowledge gap, impeding the accurate assessment of efficacy, safety, and appropriate dosage. The observed effects of botanical compounds in vitro or in animal models do not reliably translate to human clinical outcomes. For example, a plant extract demonstrating anti-inflammatory properties in laboratory settings may fail to exhibit the same effect in patients with rheumatoid arthritis due to differences in bioavailability, metabolism, or the complexity of the human immune system. The disparity between preclinical findings and clinical validation constitutes a significant obstacle in determining the true value of plant-based interventions.
Further compounding the issue is the lack of standardization in herbal products. Variations in plant species, growing conditions, harvesting methods, and extraction processes can lead to significant differences in the composition and potency of herbal preparations. This variability makes it difficult to replicate study results and to determine the optimal dosage for achieving consistent therapeutic effects. A patient using the same botanical name from different sources may inadvertently receive a product with varying levels of active compounds, potentially leading to unpredictable outcomes or adverse reactions. The absence of robust quality control measures and standardized manufacturing practices further exacerbates the challenge of scientific validation.
In conclusion, the reliance on anecdotal evidence and traditional use without adequate scientific validation poses a considerable risk to patients seeking plant-derived treatments for rheumatoid arthritis. Addressing the scientific validation gaps requires a concerted effort to conduct well-designed, randomized, controlled clinical trials using standardized herbal products. Until such evidence is available, the claims of a definitive plant-derived treatment for rheumatoid arthritis remain speculative and warrant cautious skepticism. The pursuit of rigorous scientific validation is essential to ensure patient safety, inform clinical decision-making, and ultimately determine the true therapeutic potential of botanical remedies for this chronic inflammatory disease.
4. Individual variability effects
The potential for botanical interventions in rheumatoid arthritis is significantly modulated by individual variability. The response to any therapeutic agent, including those derived from plants, is not uniform across all individuals. Intrinsic biological factors and external influences contribute to this heterogeneity, impacting the efficacy and safety of the proposed remedy. Understanding these sources of variation is crucial for a responsible and informed approach to utilizing plant-based treatments for rheumatoid arthritis.
- Genetic Predisposition
Genetic factors influence immune system function, inflammatory responses, and drug metabolism. Polymorphisms in genes encoding drug-metabolizing enzymes, such as cytochrome P450s, can alter the rate at which an individual processes herbal compounds, affecting both their efficacy and potential toxicity. Similarly, variations in genes related to immune regulation can influence the susceptibility to autoimmune diseases and the response to anti-inflammatory agents. Consequently, individuals with different genetic profiles may exhibit varying degrees of benefit or harm from the same botanical remedy.
- Gut Microbiome Composition
The gut microbiome plays a vital role in modulating immune function and inflammation. The composition and diversity of gut bacteria can influence the bioavailability and metabolism of herbal compounds, as well as the overall inflammatory milieu in the body. Individuals with distinct gut microbiome profiles may exhibit differing responses to plant-derived substances, with some experiencing enhanced therapeutic effects while others experience limited or adverse outcomes. The gut microbiota’s involvement in modulating inflammation and drug metabolism necessitates consideration in the context of botanical interventions.
- Co-existing Medical Conditions
The presence of other medical conditions can influence the response to herbal remedies. For example, individuals with impaired liver or kidney function may exhibit altered metabolism and excretion of herbal compounds, increasing the risk of toxicity. Co-existing autoimmune diseases or chronic inflammatory conditions can also modify the immune response to plant-derived substances, potentially leading to unexpected interactions or reduced efficacy. A comprehensive assessment of an individual’s medical history is essential before initiating any botanical treatment to mitigate potential risks associated with co-morbidities.
- Lifestyle Factors
Lifestyle factors, such as diet, exercise, and smoking habits, can impact the overall inflammatory state of the body and the effectiveness of herbal remedies. Dietary choices can influence gut microbiome composition and inflammatory pathways, potentially modifying the response to anti-inflammatory herbal compounds. Regular exercise can enhance immune function and reduce inflammation, potentially synergizing with the effects of botanical interventions. Conversely, smoking can exacerbate inflammation and impair immune function, potentially negating the benefits of plant-derived treatments. Modification of lifestyle factors represents an integral component of a holistic approach to managing rheumatoid arthritis and optimizing the response to botanical remedies.
These facets underscore the critical importance of considering individual variability when evaluating the potential of botanical interventions for rheumatoid arthritis. The absence of a universal response necessitates a personalized approach, taking into account genetic predisposition, gut microbiome composition, co-existing medical conditions, and lifestyle factors. A comprehensive assessment of these variables, coupled with careful monitoring and collaboration with healthcare professionals, is essential to ensure the safe and effective use of plant-based remedies in managing this complex autoimmune disease. The inherent complexity of biological systems dictates that a standardized herbal “cure” applicable to all individuals is unlikely, and a more nuanced, personalized approach is warranted.
5. Safety profile concerns
The intersection of plant-derived interventions and rheumatoid arthritis management is significantly marked by safety considerations. The widespread perception of botanical remedies as inherently safe overlooks the potential for adverse effects, drug interactions, and variations in product quality. The assumption that “natural” equates to “safe” is a fallacy that can lead to patient harm, especially in the context of a chronic autoimmune disease requiring careful and continuous medical supervision. One significant concern arises from the lack of standardization in herbal products. Variations in plant species, growing conditions, harvesting techniques, and extraction methods can lead to inconsistencies in the composition and potency of herbal preparations. This variability can result in unpredictable therapeutic effects and an increased risk of adverse reactions. For example, two different batches of a particular herbal extract may contain markedly different concentrations of the active compounds, leading to either inefficacy or toxicity.
Another critical aspect is the potential for herb-drug interactions. Many plant-derived substances can interact with conventional pharmaceuticals, altering their pharmacokinetic or pharmacodynamic properties. These interactions can lead to decreased drug efficacy, increased drug toxicity, or unexpected side effects. For instance, St. John’s Wort, a commonly used herbal antidepressant, is known to interact with several medications, including immunosuppressants used in the treatment of rheumatoid arthritis. This interaction can potentially reduce the effectiveness of the immunosuppressant, leading to a flare-up of the autoimmune disease. Furthermore, some botanical remedies may have inherent toxicities. Certain plants contain compounds that can cause liver damage, kidney damage, or other organ system dysfunctions. The long-term use of such remedies can pose a significant risk to patients with rheumatoid arthritis, who may already be vulnerable due to the disease itself or the side effects of conventional medications.
In summary, safety profile concerns represent a critical challenge in the evaluation and application of plant-derived treatments for rheumatoid arthritis. The lack of standardization, the potential for herb-drug interactions, and the presence of inherent toxicities necessitate a cautious and evidence-based approach. Patients considering herbal remedies should consult with qualified healthcare professionals to assess potential risks and benefits and to ensure that the chosen interventions are safe and appropriate. Rigorous quality control measures, standardized manufacturing practices, and comprehensive clinical trials are essential to address these concerns and to establish the true safety profile of botanical treatments for rheumatoid arthritis.
6. Integration challenges
The incorporation of plant-derived substances into the treatment paradigm for rheumatoid arthritis presents notable integration challenges. These challenges stem from various factors, including a lack of comprehensive scientific evidence, potential interactions with conventional medications, and difficulties in standardization and quality control. The interaction between herbal remedies and pharmaceutical interventions poses a substantial obstacle, influencing the effectiveness and safety of treatment. For instance, combining certain botanical compounds with immunosuppressant drugs may result in diminished efficacy of the pharmaceutical agent or, conversely, heightened toxicity. A patient concurrently utilizing methotrexate, a common disease-modifying antirheumatic drug (DMARD), and specific herbal supplements could experience unpredictable fluctuations in drug levels or synergistic adverse effects, thereby complicating disease management. Moreover, the absence of stringent regulatory oversight in the herbal supplement industry further exacerbates these challenges. Inconsistent manufacturing practices can lead to variations in product potency and purity, creating uncertainty regarding the appropriate dosage and potentially exposing patients to contaminants or adulterants.
The standardization of herbal preparations remains a significant hurdle. Unlike conventional pharmaceuticals, where precise dosages and manufacturing processes are strictly regulated, herbal products often exhibit considerable variability in their composition and concentration of active constituents. This lack of standardization makes it difficult to determine the optimal dosage for achieving therapeutic effects and to replicate research findings across different studies. A comparative analysis of different brands of the same herbal supplement might reveal substantial disparities in the quantity of the active ingredient, thereby rendering dosage recommendations unreliable and hindering the development of evidence-based guidelines. Practical application of plant-derived remedies in rheumatoid arthritis management, therefore, necessitates a cautious and individualized approach, informed by a thorough understanding of potential interactions and limitations.
In summary, the integration of herbal substances into rheumatoid arthritis treatment faces numerous challenges rooted in scientific uncertainty, potential drug interactions, and difficulties in standardization. Addressing these challenges requires a collaborative effort involving healthcare professionals, researchers, and regulatory agencies. Enhanced research into the efficacy and safety of herbal remedies, coupled with stricter quality control measures and standardized manufacturing practices, is essential to ensure the responsible and effective integration of these therapies into the conventional treatment paradigm for rheumatoid arthritis.
Frequently Asked Questions Regarding Plant-Derived Remedies for Rheumatoid Arthritis
The following addresses common inquiries concerning the potential use of plant-derived substances in the management of rheumatoid arthritis. Information is presented in a factual and objective manner, emphasizing the current state of scientific knowledge.
Question 1: Are plant-based substances capable of completely eradicating rheumatoid arthritis?
Currently, there is no scientific evidence to support the claim that any plant-derived substance can completely eradicate rheumatoid arthritis. The disease is a chronic autoimmune disorder, and available treatments, including conventional pharmaceuticals and complementary therapies, primarily focus on managing symptoms and slowing disease progression.
Question 2: What are the commonly used plant-based interventions for rheumatoid arthritis?
Certain botanicals, such as turmeric (curcumin), ginger, boswellia, and willow bark, have been investigated for their potential anti-inflammatory and analgesic properties in the context of rheumatoid arthritis. However, the level of scientific evidence supporting their efficacy varies, and further research is often warranted.
Question 3: Are herbal remedies safe for all individuals with rheumatoid arthritis?
The safety of herbal remedies is not guaranteed for all individuals. Plant-derived substances can interact with conventional medications, potentially altering their effectiveness or increasing the risk of adverse effects. Pre-existing medical conditions, such as liver or kidney dysfunction, can also influence the metabolism and excretion of herbal compounds, increasing the risk of toxicity. Consultation with a qualified healthcare professional is essential before initiating any herbal treatment.
Question 4: How can the quality and purity of herbal products be ensured?
Ensuring the quality and purity of herbal products can be challenging due to the lack of stringent regulatory oversight in the herbal supplement industry. It is advisable to procure herbal products from reputable suppliers that adhere to Good Manufacturing Practices (GMP). Look for products that have been independently tested for quality and purity. However, even with these precautions, variability in product composition remains a concern.
Question 5: Should plant-based remedies be used as a substitute for conventional medical treatment?
Plant-based remedies should not be used as a substitute for conventional medical treatment for rheumatoid arthritis. Conventional treatments, such as disease-modifying antirheumatic drugs (DMARDs) and biologics, have been proven to be effective in slowing disease progression and preventing joint damage. Herbal remedies may be considered as complementary therapies to help manage symptoms, but they should be integrated into a comprehensive treatment plan under the supervision of a healthcare professional.
Question 6: Where can reliable information about plant-based remedies for rheumatoid arthritis be found?
Reliable information about plant-based remedies can be found in peer-reviewed scientific journals, reputable herbal medicine databases, and resources provided by healthcare organizations. It is crucial to critically evaluate the information and to consult with a qualified healthcare professional for personalized advice.
In summary, while some plant-derived substances may offer potential benefits in managing rheumatoid arthritis symptoms, they should not be considered a replacement for conventional medical care. A cautious and informed approach, involving consultation with healthcare professionals and a critical evaluation of scientific evidence, is essential to ensure patient safety and optimize treatment outcomes.
The subsequent section will delve into potential future avenues of research related to plant-based interventions for rheumatoid arthritis.
Concerning Plant-Based Treatments for Rheumatoid Arthritis
This exploration has critically examined the concept of a direct “herbal cure for rheumatoid arthritis.” The analysis reveals that while certain botanical substances exhibit anti-inflammatory and analgesic properties, the evidence supporting their ability to fundamentally alter the course of this chronic autoimmune disease remains limited. The existing scientific literature highlights significant gaps in validation, standardization challenges, and potential safety concerns that must be carefully considered. The notion of a straightforward plant-derived solution lacks the robust scientific backing necessary to warrant its endorsement as a primary treatment modality.
Therefore, a measured and evidence-based perspective is essential. Individuals seeking alternative or complementary approaches to rheumatoid arthritis management are strongly encouraged to prioritize consultation with qualified healthcare professionals. Further research is crucial to elucidate the true therapeutic potential, mechanisms of action, and safety profiles of specific botanical interventions. A collaborative approach, integrating conventional medical care with carefully selected and monitored plant-based therapies, may offer some benefit in symptom management, but should not be viewed as a replacement for established and proven treatments. Until more rigorous scientific data becomes available, the concept of a definitive “herbal cure for rheumatoid arthritis” remains an aspiration, not a scientifically validated reality.