The phrase refers to the use of botanical substances in attempts to treat or alleviate the symptoms of tuberculosis, a disease caused by the bacterium Mycobacterium tuberculosis. It represents an approach that explores natural sources as alternatives or complements to conventional medical treatments for this infectious condition. Such approaches are often rooted in traditional medicine practices across various cultures.
Historically, plant-derived remedies have played a significant role in addressing a wide spectrum of ailments, including respiratory infections. The appeal of utilizing naturally sourced compounds stems from their perceived accessibility, potential for fewer adverse effects compared to pharmaceutical drugs, and integration within holistic healthcare beliefs. However, it is essential to consider these approaches within the framework of established scientific research and clinical validation.
The subsequent discussion will delve into the scientific evidence, regulatory considerations, and potential risks associated with the use of plant-based therapies for tuberculosis. It will also explore the current state of research and the importance of consulting qualified healthcare professionals before considering such options.
Guidance Regarding Plant-Based Approaches to Tuberculosis
The following information is presented to foster understanding of the complexities surrounding botanical substances as a therapeutic avenue for tuberculosis. It is imperative to approach this topic with caution, prioritizing scientific evidence and professional medical guidance above anecdotal claims.
Tip 1: Consult a Qualified Healthcare Professional: Prior to considering any plant-based remedy, a comprehensive evaluation by a physician specializing in pulmonary diseases or infectious diseases is essential. This ensures accurate diagnosis and appropriate treatment based on established medical protocols.
Tip 2: Understand the Limitations: Current scientific evidence supporting the efficacy of plant-derived treatments as a standalone cure for tuberculosis is limited. Conventional antibiotic therapy remains the cornerstone of treatment and should not be abandoned in favor of unproven alternatives.
Tip 3: Research Potential Interactions: Many botanical substances can interact with conventional medications, potentially altering their effectiveness or increasing the risk of adverse effects. Informing a healthcare provider of all supplements and herbs being taken is crucial.
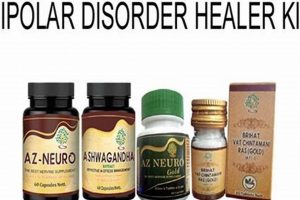
Tip 4: Verify Product Quality: The quality and composition of herbal products can vary significantly. Look for reputable brands that adhere to good manufacturing practices and provide third-party testing for purity and potency.
Tip 5: Be Aware of Potential Side Effects: Plant-derived remedies are not inherently safe. Certain herbs can cause adverse reactions, especially in individuals with pre-existing health conditions. Monitor for any unusual symptoms and seek medical attention if necessary.
Tip 6: Approach Anecdotal Evidence with Skepticism: Personal testimonials should not be considered a substitute for scientific evidence. Clinical trials and rigorous research are needed to determine the true effectiveness of any treatment.
Tip 7: Maintain Open Communication with Healthcare Providers: Transparency and open communication with healthcare providers are paramount. Disclose all treatment choices, including complementary therapies, to ensure coordinated and safe care.
Prioritizing scientifically validated treatments, coupled with informed decision-making and consultation with medical professionals, is vital when addressing tuberculosis. The integration of botanical substances should only be considered within the framework of comprehensive and evidence-based medical care.
The subsequent sections will address the regulatory landscape and scientific research currently being conducted in this complex area.
1. Limited Scientific Validation
The concept of “limited scientific validation” forms a critical backdrop when evaluating the viability of botanical approaches to tuberculosis (TB). Its relevance centers on the understanding that traditional use or anecdotal evidence does not equate to proven efficacy and safety based on modern scientific standards. This deficiency necessitates a cautious approach to plant-based treatments for TB.
- Lack of Randomized Controlled Trials
The most rigorous method for evaluating medical interventions is the randomized controlled trial (RCT). Many plant-based treatments lack robust RCTs demonstrating their effectiveness against Mycobacterium tuberculosis in human subjects. The absence of such trials introduces uncertainty regarding clinical benefits and optimal dosages.
- Inadequate Standardization of Herbal Preparations
Plant-derived remedies often suffer from inconsistencies in their composition. Variations in plant species, growing conditions, harvesting methods, and extraction processes can lead to significant differences in the concentration of active compounds. This lack of standardization complicates the interpretation of research findings and hinders the establishment of reliable dosage guidelines.
- Difficulties in Isolating Active Compounds
Complex mixtures of compounds characterize many botanical substances, making it challenging to identify the specific constituents responsible for any observed therapeutic effects. Identifying, isolating, and testing these individual compounds are necessary steps to understand the mechanism of action and potential toxicity of the plant-based treatment. This isolation process is often incomplete, creating a gap in scientific understanding.
- Insufficient Data on Long-Term Safety and Efficacy
Even if short-term benefits are observed, the long-term safety and efficacy of plant-based treatments for TB remain largely unknown. Chronic use of certain herbs can lead to unexpected adverse effects or interactions with other medications. The limited availability of longitudinal studies poses a challenge to assessing the overall risk-benefit profile of these approaches.
Collectively, the lack of comprehensive scientific validation necessitates a critical assessment of “herbal cure for tb”. These factors highlight the need for prospective patients to primarily engage with evidence-based medical treatments and to consult with qualified healthcare professionals before considering plant-derived remedies. Ongoing research, adhering to rigorous scientific standards, is essential to determine the potential role of botanical substances in the future management of tuberculosis.
2. Potential Drug Interactions
The concurrent use of botanical substances, often associated with the concept of a purported “herbal cure for tb,” introduces the significant risk of potential drug interactions. This risk arises from the complex chemical compositions of many plant-derived remedies and their ability to affect drug metabolism, absorption, distribution, or excretion. Such interactions can diminish the effectiveness of conventional tuberculosis medications or, conversely, amplify their toxicity, potentially leading to severe adverse events. For instance, some herbs may induce or inhibit cytochrome P450 enzymes, a family of enzymes crucial for metabolizing many pharmaceuticals, including certain anti-tuberculosis drugs like rifampicin.
The absence of rigorous standardized testing for interactions between specific anti-tuberculosis drugs and commonly used herbs exacerbates the potential for harm. Many individuals pursuing alternative or complementary therapies may not fully disclose their use of botanical substances to their healthcare providers, further complicating the management of their condition. Cases have been reported where patients on tuberculosis treatment experienced liver damage or treatment failure due to the undisclosed use of herbal remedies that interfered with the metabolism of their prescribed medications. Therefore, a thorough assessment of potential interactions is crucial before combining any botanical substance with conventional anti-tuberculosis therapy.
In summary, the risk of drug interactions represents a significant challenge to the safe and effective integration of plant-derived substances into the treatment regimen for tuberculosis. A comprehensive understanding of these interactions, proactive disclosure by patients, and careful monitoring by healthcare professionals are essential to mitigate the potential for adverse outcomes. Emphasis should be placed on prioritizing evidence-based treatment protocols and avoiding the unverified combination of herbal remedies with essential tuberculosis medications.
3. Varied Product Quality
The inconsistent quality of botanical products sold under the premise of providing relief or a purported “herbal cure for tb” presents a significant challenge to individuals seeking alternative treatments. This variability stems from a lack of stringent regulatory oversight, inconsistencies in manufacturing processes, and deceptive marketing practices. The consequences of such inconsistencies can range from a complete lack of therapeutic benefit to serious adverse health effects.
- Source Material Authentication
The accurate identification and authentication of plant species are paramount. Adulteration, substitution with inferior or toxic species, and mislabeling are common occurrences in the herbal product industry. Without proper verification, consumers cannot be certain that the product contains the intended ingredients or that it is free from contaminants. This raises serious concerns when a product is promoted as a tuberculosis treatment, as the patient’s health could be compromised by ineffective or harmful substances.
- Cultivation and Harvesting Practices
Environmental factors, cultivation methods, and harvesting techniques significantly influence the chemical composition and potency of medicinal plants. Variations in soil quality, sunlight exposure, and harvesting time can alter the levels of active compounds. Poor agricultural practices, such as the use of pesticides or heavy metals, can contaminate the final product, posing a health risk to consumers. The impact of these inconsistencies is amplified when patients rely on these products for managing a serious condition like tuberculosis.
- Extraction and Manufacturing Processes
The methods used to extract active compounds from plant materials and formulate them into final products can affect their bioavailability and stability. Inadequate or improper extraction techniques may result in low concentrations of active compounds, rendering the product ineffective. Furthermore, the use of inappropriate solvents or excipients can introduce contaminants or compromise product safety. A lack of standardized manufacturing processes and quality control measures can lead to significant batch-to-batch variations, making it difficult to ensure consistent therapeutic outcomes for tuberculosis patients.
- Lack of Regulatory Oversight
The regulatory framework governing herbal products varies widely across different countries and regions. In many jurisdictions, herbal products are classified as dietary supplements rather than pharmaceuticals, subjecting them to less stringent quality control and marketing requirements. This lack of regulatory oversight allows manufacturers to make unsubstantiated claims about product efficacy and safety, without providing scientific evidence to support their assertions. The absence of robust regulatory mechanisms increases the risk of consumers being misled by deceptive marketing practices and purchasing substandard or adulterated products marketed as a solution for tuberculosis.
Collectively, these factors underscore the inherent risks associated with the varied product quality of herbal preparations marketed as a “herbal cure for tb.” Patients seeking treatment for tuberculosis should prioritize evidence-based medical care and consult with qualified healthcare professionals to ensure the appropriate management of their condition. The inconsistent quality of herbal products undermines their potential therapeutic benefits and may pose serious health risks, highlighting the need for greater regulatory scrutiny and consumer awareness.
4. Accessibility and Affordability
The perceived accessibility and affordability of botanical remedies are often cited as reasons for their consideration in the management of tuberculosis, particularly in resource-limited settings. This perception stems from a confluence of factors, including the ready availability of certain plants, lower costs compared to pharmaceutical interventions, and the integration of herbal medicine within traditional healthcare systems. However, this view overlooks several critical complexities regarding efficacy, safety, and the true economic burden of relying solely on unproven botanical treatments.
- Geographical Availability and Traditional Knowledge
In many regions, particularly in developing countries, specific medicinal plants are locally abundant and readily accessible. Traditional knowledge regarding their use for various ailments, including respiratory conditions suggestive of tuberculosis, has been passed down through generations. This accessibility can foster a sense of self-reliance and potentially reduce the immediate financial burden associated with seeking conventional medical care. However, such reliance should be tempered by a recognition that traditional use does not equate to scientifically validated efficacy against Mycobacterium tuberculosis. The lack of rigorous diagnostic testing can lead to misdiagnosis and delayed access to appropriate treatment, potentially resulting in disease progression and increased transmission.
- Lower Upfront Costs Compared to Pharmaceuticals
The upfront cost of purchasing herbal remedies is often lower than that of acquiring a full course of anti-tuberculosis drugs. This difference can be particularly significant for individuals with limited financial resources or those living in areas with inadequate healthcare infrastructure. However, this analysis fails to account for the potential long-term costs associated with ineffective treatment. Reliance on unproven botanical substances may lead to prolonged illness, increased healthcare expenditures due to complications, and reduced productivity. Furthermore, the lack of standardized dosages and quality control can result in the consumption of ineffective or even harmful herbal products, negating any initial cost savings.
- Integration within Traditional Healthcare Systems
In some cultures, traditional medicine, including the use of herbal remedies, is deeply ingrained within the healthcare system and is often the first point of contact for individuals seeking medical care. This integration can facilitate access to treatment for those who may face barriers to accessing conventional medical services due to geographical distance, cultural beliefs, or financial constraints. However, the absence of standardized training and regulation for traditional healers raises concerns about the quality and safety of the care provided. Reliance on traditional healers without proper diagnostic testing and access to effective anti-tuberculosis drugs can lead to suboptimal treatment outcomes and contribute to the spread of the disease.
- Potential Economic Burden of Ineffective Treatment
While herbal remedies may seem affordable in the short term, the long-term economic consequences of relying on ineffective treatments for tuberculosis can be substantial. Prolonged illness can lead to reduced productivity, loss of income, and increased healthcare expenditures due to complications. Furthermore, the spread of drug-resistant tuberculosis strains due to inadequate treatment can result in more expensive and prolonged treatment regimens. A comprehensive economic analysis should consider the total cost of care, including the costs associated with ineffective treatment, complications, and the potential spread of drug-resistant strains. Prioritizing evidence-based treatment strategies and ensuring access to affordable, high-quality anti-tuberculosis drugs are essential for mitigating the economic burden of the disease.
The allure of accessible and affordable “herbal cures for tb” must be critically evaluated within the context of proven efficacy, safety, and the potential long-term economic consequences of ineffective treatment. A balanced approach should prioritize access to evidence-based medical care, while also acknowledging the role of traditional medicine within cultural contexts. Further research is needed to explore the potential synergistic effects of combining botanical substances with conventional anti-tuberculosis drugs, but such research must adhere to rigorous scientific standards and prioritize patient safety.
5. Traditional Medicine Integration
Traditional Medicine Integration, in the context of exploring a purported “herbal cure for tb,” signifies the incorporation of historically utilized plant-based remedies into established healthcare frameworks. This incorporation ranges from informal use within communities to formal recognition by national health authorities. The integration, however, presents complex challenges regarding standardization, efficacy validation, and potential interactions with conventional medical treatments.
- Cultural Acceptance and Accessibility
In numerous cultures, traditional medicine represents the primary or sole source of healthcare, particularly in rural or underserved communities. This cultural acceptance often translates to a greater willingness to utilize plant-based remedies. Accessibility, both geographically and economically, further reinforces this reliance. For example, in some regions of Asia and Africa, individuals turn to traditional healers for the management of tuberculosis symptoms due to limited access to conventional medical facilities or an inability to afford pharmaceutical treatments. The implication is that any discourse on “herbal cure for tb” must acknowledge this existing paradigm of healthcare delivery.
- Varying Degrees of Formal Recognition
The extent to which traditional medicine is formally recognized and regulated varies considerably across countries. Some nations have established regulatory bodies to oversee the practice of traditional medicine and the manufacturing of herbal products, while others lack such oversight. In China, for instance, Traditional Chinese Medicine (TCM) is integrated into the national healthcare system, with TCM practitioners working alongside conventional medical doctors. This formal integration implies a degree of standardization and quality control. Conversely, in countries where traditional medicine operates outside the purview of formal regulation, the quality, safety, and efficacy of herbal remedies remain largely unmonitored, posing potential risks to individuals seeking a so-called “herbal cure for tb.”
- Potential for Collaboration with Conventional Medicine
Opportunities exist for collaboration between traditional medicine practitioners and conventional medical providers. Such collaborations can potentially enhance patient care by combining the strengths of both approaches. For instance, traditional medicine could be utilized to manage the side effects of anti-tuberculosis drugs, while conventional medicine addresses the underlying infection. However, effective collaboration requires mutual respect, open communication, and a shared commitment to evidence-based practice. Challenges to collaboration include differing diagnostic paradigms, a lack of scientific validation for many traditional treatments, and concerns about potential drug interactions. Therefore, the integration of traditional medicine in the context of a supposed “herbal cure for tb” should not supplant conventional treatments but may, under appropriate circumstances and with proper medical oversight, serve as a complementary approach.
- Challenges in Standardization and Quality Control
One of the primary obstacles to integrating traditional medicine into mainstream healthcare is the lack of standardization and quality control for herbal products. The composition of plant-based remedies can vary significantly depending on factors such as plant species, growing conditions, harvesting methods, and extraction processes. This variability makes it difficult to determine appropriate dosages and to ensure consistent therapeutic effects. Adulteration with other herbs, heavy metals, or even pharmaceuticals is also a concern. Addressing these challenges requires the implementation of rigorous quality control measures, including standardized manufacturing processes, authentication of plant materials, and testing for contaminants. Absent such measures, the promise of a reliable “herbal cure for tb” remains elusive.
These facets collectively demonstrate the complexity surrounding the incorporation of traditional medicine, particularly in the context of a “herbal cure for tb.” Cultural acceptance, varying degrees of formal recognition, opportunities for collaboration, and challenges in standardization all shape the landscape. Any responsible exploration of botanical approaches to tuberculosis must acknowledge these factors and prioritize evidence-based medical care, while also recognizing the potential, and limitations, of traditional healing practices.
6. Complementary Role Only
The phrase “Complementary Role Only” in relation to “herbal cure for tb” denotes the understanding that botanical substances, at present, lack sufficient scientific validation to serve as a standalone cure for tuberculosis. This understanding underscores the critical need to view plant-derived remedies as adjunctive therapies that may potentially support, but not replace, conventional antibiotic treatment. The basis for this stance lies in the lack of robust clinical trials demonstrating that herbal interventions can consistently and reliably eradicate Mycobacterium tuberculosis in infected individuals. Therefore, any assertion that herbal remedies can independently cure tuberculosis should be regarded with considerable skepticism.
The emphasis on a “Complementary Role Only” is further reinforced by considering the potential for herb-drug interactions. Many botanical substances contain complex chemical compounds that can interfere with the metabolism or efficacy of conventional anti-tuberculosis drugs. For example, certain herbal preparations may induce liver enzymes that accelerate the breakdown of rifampicin, a key anti-tuberculosis medication, thereby reducing its effectiveness. In such cases, the purported benefits of the herbal remedy may be offset by a reduction in the efficacy of the conventional treatment, leading to poorer outcomes for the patient. Moreover, the inconsistent quality and standardization of herbal products further complicate their integration into tuberculosis treatment regimens. Variations in plant species, growing conditions, and extraction methods can result in significant differences in the concentration of active compounds, making it difficult to determine appropriate dosages and ensure consistent therapeutic effects.
In conclusion, the concept of “Complementary Role Only” serves as a crucial caveat when evaluating the potential of botanical substances in tuberculosis management. While certain herbs may possess properties that could alleviate symptoms or support overall well-being, they should not be considered a substitute for evidence-based medical care. The practical significance of this understanding lies in promoting responsible decision-making, prioritizing patient safety, and ensuring that individuals with tuberculosis receive appropriate and effective treatment based on established medical guidelines. Therefore, a cautious and informed approach is warranted, emphasizing the integration of herbal remedies only under the guidance and supervision of qualified healthcare professionals and as an adjunct to, not a replacement for, conventional anti-tuberculosis therapy.
Frequently Asked Questions Regarding Botanical Approaches to Tuberculosis
The following questions and answers address common concerns and misconceptions surrounding the use of plant-derived remedies in the treatment of tuberculosis (TB). The information provided is intended to offer clarity and promote informed decision-making.
Question 1: Can herbal remedies completely cure tuberculosis?
Currently, no scientific evidence supports the assertion that herbal remedies can serve as a standalone cure for tuberculosis. Conventional antibiotic therapy remains the cornerstone of treatment and should not be abandoned in favor of unproven alternatives.
Question 2: Are herbal remedies safe to use alongside conventional tuberculosis medications?
The concurrent use of herbal remedies and conventional tuberculosis medications carries the risk of potential drug interactions. Some herbs can interfere with the metabolism or efficacy of anti-tuberculosis drugs, potentially leading to adverse outcomes. Consultation with a healthcare professional is essential before combining any herbal remedy with conventional treatment.
Question 3: Are all herbal products of the same quality?
The quality of herbal products can vary significantly due to differences in plant species, growing conditions, harvesting methods, and manufacturing processes. Lack of regulatory oversight further contributes to inconsistencies in product quality. It is crucial to source herbal products from reputable manufacturers that adhere to good manufacturing practices and provide third-party testing for purity and potency.
Question 4: Is traditional use of an herb a guarantee of its effectiveness against tuberculosis?
Traditional use of an herb does not automatically equate to proven effectiveness against tuberculosis. Anecdotal evidence and historical use should not be considered a substitute for rigorous scientific research and clinical trials. The efficacy of any treatment must be validated through established scientific methods.
Question 5: Are there specific herbal remedies that have been proven effective against tuberculosis?
While some herbal remedies have demonstrated in vitro activity against Mycobacterium tuberculosis, the majority lack robust clinical evidence of effectiveness in human subjects. Limited scientific evidence necessitates caution, and the use of herbal remedies should not supplant conventional treatment.
Question 6: What should be done if someone is considering using herbal remedies for tuberculosis?
If considering the use of herbal remedies for tuberculosis, consultation with a qualified healthcare professional specializing in pulmonary diseases or infectious diseases is paramount. This ensures accurate diagnosis, appropriate treatment based on established medical protocols, and monitoring for potential drug interactions or adverse effects.
In summary, the information presented serves to emphasize the importance of evidence-based medical care and informed decision-making when addressing tuberculosis. The use of herbal remedies should be approached with caution and integrated only within the framework of comprehensive and scientifically validated medical treatment.
The subsequent section will address resources for further information and support.
Conclusion
The exploration of “herbal cure for tb” reveals a complex landscape marked by limited scientific validation, potential drug interactions, and varied product quality. While traditional medicine offers accessibility and affordability in certain regions, its integration into tuberculosis treatment demands careful consideration. Existing evidence advocates for botanical substances playing a complementary role only, not replacing established antibiotic therapies. The information presented underscores the importance of consulting healthcare professionals before pursuing any alternative treatments.
The ongoing pursuit of effective tuberculosis treatments necessitates rigorous scientific research and adherence to evidence-based practices. Further investigation into potential synergistic effects between botanical compounds and conventional medications warrants attention, but patient safety and well-being must remain paramount. A future where novel therapeutic strategies emerge relies on a commitment to robust clinical trials and the dissemination of accurate, reliable information.