Plant-derived remedies intended to manage hypertension encompass a range of natural substances. These preparations, often available in various forms such as teas, capsules, and tinctures, are utilized with the aim of reducing blood pressure levels. Examples include hawthorn, garlic, and hibiscus, each purported to possess properties that contribute to cardiovascular health.
The use of botanical treatments for elevated blood pressure dates back centuries, with traditional medicine systems worldwide incorporating plants for their perceived therapeutic effects. Interest in these alternative approaches continues due to factors like perceived gentler side effects compared to pharmaceutical interventions and a holistic approach to wellness. Scientific investigation explores the efficacy of these treatments and their potential role in complementing conventional medical care for hypertension.
The subsequent sections will delve into specific plant-based options commonly considered for managing hypertension, examining available research on their mechanisms of action, potential benefits, risks, and appropriate usage. A balanced perspective on the role of these options within a comprehensive approach to blood pressure management will also be presented.
Guidance on Plant-Based Options for Hypertension Management
The following points offer guidance regarding the use of botanical options in addressing high blood pressure. These are provided for informational purposes and do not constitute medical advice.
Tip 1: Consultation with a Healthcare Professional: Prior to initiating any plant-based regimen for hypertension, consultation with a qualified healthcare provider is imperative. A medical professional can assess individual health status, potential interactions with existing medications, and the suitability of botanical interventions.
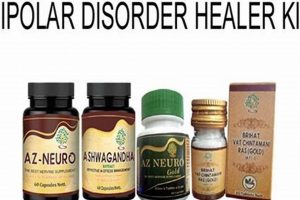
Tip 2: Research-Based Selection: Choosing options supported by scientific investigation is recommended. Review available studies and clinical trials to understand the potential benefits and limitations of specific herbs or formulations. Prioritize substances with demonstrated efficacy in blood pressure reduction.
Tip 3: Dosage and Standardization: Adhering to recommended dosages is crucial. Opt for standardized extracts whenever possible to ensure consistent levels of active compounds. Deviations from established dosage guidelines can impact effectiveness and safety.
Tip 4: Monitoring Blood Pressure Regularly: Consistent monitoring of blood pressure is necessary to evaluate the impact of plant-based interventions. Maintain a record of blood pressure readings to track progress and identify any adverse changes.
Tip 5: Awareness of Potential Interactions: Certain plants can interact with pharmaceutical medications, potentially altering their effects. Inform healthcare providers of all botanical supplements being taken to mitigate the risk of adverse interactions.
Tip 6: Lifestyle Integration: Botanical remedies are often most effective when incorporated into a broader lifestyle strategy that includes a healthy diet, regular physical activity, stress management techniques, and adequate sleep. A holistic approach to health is essential.
Tip 7: Quality Assurance: Select reputable suppliers of herbal supplements to ensure product quality and purity. Look for products that have undergone third-party testing to verify their composition and absence of contaminants.
These suggestions emphasize the importance of evidence-based decision-making, professional guidance, and responsible usage within the context of managing hypertension. A comprehensive approach that integrates both conventional and complementary modalities offers the best opportunity for positive outcomes.
The subsequent sections will provide further detail on specific options and their potential role within a comprehensive treatment plan for high blood pressure.
1. Efficacy Evidence
The connection between efficacy evidence and plant-based remedies for hypertension lies in the fundamental need to validate claims of therapeutic benefit. Without rigorous scientific investigation, the effectiveness of these remedies remains speculative. Cause-and-effect relationships between specific herbs and blood pressure reduction must be established through controlled studies. The presence of efficacy evidence is a critical component, determining whether a particular plant genuinely contributes to lowering blood pressure or merely provides a placebo effect. For example, while some studies suggest that hibiscus may have a hypotensive effect, the quality and consistency of this evidence varies, underscoring the need for further investigation.
The practical significance of understanding efficacy evidence in this context resides in informed decision-making. Individuals considering plant-based options for managing hypertension require access to reliable data that quantifies the potential benefits and risks. This information enables them to make choices aligned with their health needs and preferences, while also mitigating the possibility of ineffective or harmful treatments. Consider the case of garlic: though traditionally used to address cardiovascular concerns, varying preparations and methodologies in research complicate drawing definitive conclusions about its efficacy in consistently lowering blood pressure.
In summary, the strength of efficacy evidence directly dictates the credibility and practical applicability of any plant-based remedy for hypertension. Challenges remain in conducting adequately powered and well-designed clinical trials in this area. Continued research is necessary to provide clearer guidance on the selection, dosage, and appropriate use of herbal treatments within a comprehensive approach to managing high blood pressure, ensuring that potential benefits outweigh potential risks, and aligning with overall cardiovascular health goals.
2. Safety Profiles
The safety profiles of botanical interventions for hypertension represent a critical consideration, necessitating careful evaluation of potential adverse effects, contraindications, and individual risk factors. A comprehensive understanding of these profiles is essential for responsible and informed decision-making.
- Hepatotoxicity
Some herbs, while potentially beneficial in other respects, may exhibit hepatotoxic properties. Prolonged or excessive consumption can, in certain individuals, result in liver damage. For example, specific preparations containing pyrrolizidine alkaloids have been associated with liver toxicity. Vigilance and appropriate liver function monitoring are therefore necessary when using these remedies.
- Nephrotoxicity
Certain plant constituents possess the potential to induce kidney damage, particularly in individuals with pre-existing renal conditions. Aristolochic acids, found in some herbal products, have been linked to nephropathy and renal failure. Strict avoidance of products containing these substances is paramount.
- Allergic Reactions
Hypersensitivity reactions to botanical substances are not uncommon. These reactions can range from mild skin irritation to severe anaphylaxis. Individuals with known allergies to plants should exercise caution and initiate use of new herbal remedies with small test doses.
- Interactions with Medications
Many plants contain bioactive compounds that can interact with pharmaceutical medications, potentially altering their pharmacokinetic or pharmacodynamic effects. St. John’s Wort, for example, is known to induce cytochrome P450 enzymes, affecting the metabolism of numerous drugs. Consideration of potential interactions is essential when combining herbal and conventional treatments.
The overall safety profile of botanical treatments for high blood pressure depends heavily on the specific plant, the preparation method, dosage, and individual health status. A thorough assessment of these factors, in consultation with a qualified healthcare provider, is necessary to minimize risks and ensure responsible use of these interventions within a comprehensive approach to hypertension management.
3. Drug Interactions
The potential for interactions between botanical remedies and pharmaceutical medications represents a significant concern in the management of hypertension. These interactions can alter the efficacy or toxicity of either the herbal product or the conventional drug, leading to unintended and potentially adverse consequences. Careful consideration and professional oversight are essential.
- Pharmacokinetic Interactions
Pharmacokinetic interactions involve alterations in the absorption, distribution, metabolism, or excretion of a drug. Certain herbs can influence the activity of cytochrome P450 enzymes in the liver, which play a crucial role in metabolizing many pharmaceutical medications. For example, St. John’s Wort, known for its antidepressant properties, induces CYP3A4, accelerating the metabolism of drugs like warfarin, potentially reducing their effectiveness and increasing the risk of thromboembolic events. Conversely, other herbs may inhibit these enzymes, leading to increased drug concentrations and potential toxicity. Grapefruit juice, though not strictly an herb, exemplifies this phenomenon, inhibiting CYP3A4 and increasing the levels of certain statins and calcium channel blockers.
- Pharmacodynamic Interactions
Pharmacodynamic interactions occur when two or more substances have additive, synergistic, or antagonistic effects on the body. Combining herbal remedies with similar mechanisms of action as conventional antihypertensive drugs can lead to excessive blood pressure reduction, resulting in hypotension. For instance, concurrent use of hawthorn (Crataegus spp.) with ACE inhibitors or beta-blockers may potentiate the hypotensive effect, increasing the risk of dizziness, lightheadedness, or even syncope. Conversely, some herbs may antagonize the effects of antihypertensive drugs, rendering them less effective. Licorice root, for example, contains glycyrrhizin, which can cause sodium and water retention, potentially increasing blood pressure and counteracting the effects of antihypertensive medications.
- Interactions Affecting Electrolyte Balance
Certain herbal remedies possess diuretic properties, promoting fluid and electrolyte excretion. Concurrent use of these herbs with conventional diuretics can lead to excessive electrolyte depletion, particularly potassium. Potassium depletion can increase the risk of cardiac arrhythmias, especially in individuals taking digoxin. Similarly, the combined use of herbal and pharmaceutical diuretics may exacerbate dehydration and electrolyte imbalances in individuals with renal insufficiency.
- Interactions with Anticoagulants and Antiplatelet Agents
Many herbs possess inherent anticoagulant or antiplatelet properties. Combining these herbs with conventional anticoagulants like warfarin or antiplatelet agents like aspirin or clopidogrel can increase the risk of bleeding. Examples of herbs with anticoagulant or antiplatelet activity include garlic, ginger, ginkgo biloba, and ginseng. Patients taking these medications should exercise caution and consult with a healthcare professional before using these herbs to mitigate the risk of bleeding complications.
The complexity of potential drug interactions necessitates careful evaluation and individualized management. Patients should inform their healthcare providers of all herbal remedies and supplements they are using, along with their conventional medications. Healthcare professionals can then assess the risk of potential interactions and provide appropriate guidance. Monitoring for signs and symptoms of adverse effects is crucial. Furthermore, evidence-based information resources should be consulted to identify and manage potential drug interactions. A collaborative approach involving both patients and healthcare providers is essential to ensure the safe and effective use of both herbal remedies and conventional medications in the management of hypertension.
4. Dosage Standardization
Dosage standardization represents a critical challenge and necessity in the context of plant-derived remedies for hypertension. The variability inherent in plant composition and preparation methods directly impacts therapeutic efficacy and safety. Consistent and reliable dosing is essential to achieving desired clinical outcomes while minimizing the risk of adverse events.
- Variability in Plant Material
The concentration of active compounds within a single plant species can fluctuate due to factors such as growing conditions, harvesting time, and geographical location. This inherent variability presents a significant obstacle to consistent dosing. For example, the allicin content in garlic, a compound associated with blood pressure reduction, can differ substantially depending on the cultivar and processing methods. Without standardization, consumers may inadvertently receive significantly different doses of the active constituents, leading to unpredictable therapeutic effects.
- Extraction and Processing Methods
The methods employed to extract and process plant material into herbal remedies can profoundly influence the final concentration and bioavailability of active compounds. Extraction techniques using different solvents (e.g., water, ethanol) can selectively extract certain constituents, altering the overall chemical profile and therapeutic properties of the product. Inconsistent or poorly controlled processing can also degrade active compounds, diminishing the potency of the remedy. For example, improper drying of hawthorn berries can result in the loss of flavonoids, which are believed to contribute to its cardiovascular benefits.
- Standardized Extracts
Standardized extracts represent an effort to address the variability in plant material and processing by ensuring that the final product contains a specified amount of one or more active constituents. These extracts are typically assayed to quantify the concentration of marker compounds, allowing for more consistent dosing. For example, a standardized extract of Ginkgo biloba might contain a guaranteed percentage of ginkgo flavone glycosides and terpene lactones. However, it’s important to note that even standardized extracts may not capture the full spectrum of bioactive compounds present in the whole plant, and the therapeutic effects may depend on synergistic interactions between multiple constituents.
- Dosage Forms and Bioavailability
The dosage form of a herbal remedy can influence the rate and extent of absorption of active compounds into the bloodstream. Factors such as particle size, solubility, and the presence of excipients can affect bioavailability. For example, encapsulated powders may have different absorption rates compared to liquid extracts or tinctures. The method of administration (e.g., oral, topical) also plays a role. Inconsistent bioavailability can contribute to variations in therapeutic response, even when using standardized extracts. Therefore, careful consideration of the dosage form and its impact on bioavailability is crucial.
In summary, dosage standardization is paramount for ensuring the safety and efficacy of plant-derived remedies for hypertension. The variability in plant material, extraction methods, and dosage forms presents ongoing challenges. While standardized extracts offer a means of achieving more consistent dosing, it’s important to recognize their limitations and consider the potential role of other bioactive compounds. Ultimately, professional guidance and evidence-based information are essential for individuals considering botanical interventions for managing high blood pressure.
5. Professional Guidance
The intersection of professional guidance and herbal remedies for hypertension is characterized by a critical need for informed decision-making and risk mitigation. Self-prescription of herbal treatments, without the supervision of qualified healthcare personnel, may lead to adverse outcomes due to potential misdiagnosis, inappropriate selection of remedies, incorrect dosage, and unforeseen interactions with conventional medications or pre-existing medical conditions. The consultation with physicians, pharmacists, or trained herbalists provides patients with a comprehensive assessment of their health status, enabling the safe and effective integration of plant-based therapies into their overall treatment plan. For instance, a patient with uncontrolled hypertension considering the use of garlic supplements should be evaluated for potential bleeding risks, especially if concurrently taking anticoagulant medications. Professional guidance, in this scenario, facilitates the identification and management of these risks.
Considerations within professional guidance extend beyond immediate safety concerns to encompass the selection of high-quality herbal products and the monitoring of treatment efficacy. The herbal supplement market is often unregulated, leading to inconsistencies in product quality and labeling accuracy. A healthcare provider can advise patients on reputable brands and sources of herbal remedies, ensuring the purchase of products that have undergone third-party testing for purity and potency. Furthermore, ongoing monitoring of blood pressure levels is essential to determine the effectiveness of herbal interventions. Adjustments to dosage or the selection of alternative therapies may be necessary, and such decisions should be guided by healthcare professionals based on objective clinical data. The practical application of this principle is evident in cases where patients experience limited or no improvement in blood pressure despite consistent use of an herbal remedy; professional guidance allows for timely adjustments to the therapeutic approach, preventing prolonged periods of uncontrolled hypertension.
In summary, professional guidance forms an indispensable component of the responsible use of plant-based remedies for hypertension. Its role encompasses risk assessment, product selection, and treatment monitoring, thereby promoting patient safety and optimizing therapeutic outcomes. Challenges persist in ensuring widespread access to qualified healthcare providers and evidence-based information on herbal medicine. Continued efforts to integrate complementary and alternative medicine into conventional healthcare settings are necessary to facilitate the informed and safe utilization of herbal therapies in the management of hypertension and other chronic health conditions.
Frequently Asked Questions
The following questions address common concerns and misconceptions regarding plant-derived remedies for managing hypertension. These responses are intended to provide informational clarity and should not substitute professional medical advice.
Question 1: Are plant-based options a suitable replacement for conventional hypertension medications?
Plant-based options are generally not considered a direct replacement for prescription hypertension medications. While some may offer modest blood pressure reductions, their efficacy often differs from that of pharmaceutical interventions. Plant-derived remedies may complement conventional treatments but should not be used as a sole strategy without medical supervision.
Question 2: What are the potential risks associated with utilizing plant-based options for high blood pressure?
Potential risks include adverse reactions, interactions with prescription medications, and ineffective blood pressure control. Certain plant constituents can exert potent physiological effects, necessitating careful consideration of individual health conditions and concurrent treatments. Unmonitored use may result in complications or delayed access to appropriate medical care.
Question 3: How can the quality and safety of herbal supplements be ensured?
Quality and safety can be enhanced by selecting products from reputable manufacturers that adhere to Good Manufacturing Practices (GMP). Look for supplements that have undergone third-party testing for purity and potency. Verify that the product label accurately reflects the ingredients and dosage. Consultation with a healthcare professional can help identify reliable sources.
Question 4: Is there scientific evidence supporting the effectiveness of plant-derived remedies for hypertension?
Scientific evidence varies depending on the specific plant-derived remedy in question. Some options, such as hibiscus and garlic, have demonstrated some degree of efficacy in clinical trials. However, the quality and consistency of this evidence may be limited. Further research is often needed to confirm these findings and establish optimal dosages.
Question 5: What role does lifestyle modification play in managing hypertension alongside plant-based interventions?
Lifestyle modification is a cornerstone of hypertension management. A healthy diet, regular physical activity, stress management techniques, and adequate sleep are essential components. Plant-based interventions are typically most effective when integrated into a comprehensive lifestyle approach, rather than relied upon as a standalone solution.
Question 6: How does one determine the appropriate dosage of a plant-derived remedy for high blood pressure?
Determining the appropriate dosage requires careful consideration of individual factors, including age, weight, health status, and concurrent medications. It is strongly advised that a healthcare professional or qualified herbalist be consulted to establish a safe and effective dosage regimen. Adhering to recommended dosages and monitoring blood pressure levels are crucial.
The above questions and answers emphasize the need for a balanced and cautious approach to using plant-derived remedies for hypertension. Professional guidance and evidence-based information are vital to ensure both safety and efficacy.
Conclusion
The examination of herbal meds for high blood pressure reveals a complex landscape. While certain botanical options offer potential benefits in managing hypertension, their efficacy and safety profiles necessitate rigorous scrutiny. Evidence-based decision-making, guided by healthcare professionals, remains paramount. The unregulated nature of the herbal supplement market further underscores the importance of cautious product selection and adherence to established dosage guidelines.
The future utility of plant-derived remedies in addressing hypertension hinges on continued scientific investigation, standardization of preparations, and integration within conventional medical paradigms. It is crucial to approach the use of herbal interventions with a critical and informed perspective, prioritizing patient safety and well-being. Failure to do so may compromise health outcomes and undermine the responsible management of this prevalent cardiovascular condition.