The phrase refers to the employment of plant-derived substances to address Human Papillomavirus infections. This encompasses a variety of botanical remedies purported to either boost the immune system’s ability to clear the virus, or directly interfere with viral replication. Formulations can include teas, topical applications, and dietary supplements.
Interest stems from the potential for more accessible and potentially gentler therapeutic options compared to conventional medical treatments. Historically, herbal remedies have been employed across cultures for various ailments, including viral infections. The appeal lies in the perception of natural alternatives offering fewer side effects and holistic support for overall health, although rigorous scientific validation remains a critical aspect.
The subsequent sections delve into the specific plants often associated with such approaches, examining the evidence supporting their use, and considering the necessary precautions and limitations in their application.
Guidance Regarding Botanical Interventions for HPV
The following points provide essential information when exploring plant-based options to manage Human Papillomavirus infections. It is vital to approach this subject with caution and prioritize evidence-based practices.
Tip 1: Consult a Healthcare Professional: Prior to initiating any herbal regimen, seek guidance from a qualified physician or healthcare provider. This ensures the appropriateness of the selected herbs and avoids potential interactions with existing medications or medical conditions.
Tip 2: Research Specific Herbs Thoroughly: Examine the scientific literature pertaining to individual herbs of interest. Reputable sources, such as peer-reviewed journals and government health agencies, offer valuable insights into efficacy and safety profiles.
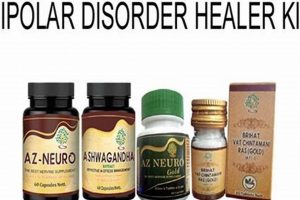
Tip 3: Source Products from Reputable Suppliers: Exercise diligence in selecting suppliers of herbal products. Opt for companies that adhere to Good Manufacturing Practices (GMP) and provide verifiable Certificates of Analysis (COAs) to confirm purity and potency.
Tip 4: Adhere to Recommended Dosages: Follow the dosage instructions provided by the healthcare provider or the product label. Exceeding recommended dosages does not necessarily enhance efficacy and may increase the risk of adverse effects.
Tip 5: Monitor for Adverse Reactions: Pay close attention to any potential side effects or allergic reactions. Discontinue use immediately and consult a healthcare professional if any unexpected symptoms arise.
Tip 6: Recognize Limitations: Understand that botanical interventions are not universally effective and may not be a substitute for conventional medical treatments. Regular screening and medical monitoring remain essential for managing HPV.
Tip 7: Focus on Immune System Support: While certain herbs may possess antiviral properties, a holistic approach that strengthens the immune system is crucial. This includes maintaining a balanced diet, engaging in regular exercise, and managing stress.
Adherence to these guidelines promotes a more informed and safer approach to exploring the potential role of plant-based remedies in managing HPV. Prioritizing evidence, professional guidance, and careful monitoring remains paramount.
The subsequent sections will offer a broader perspective on the overall management of HPV infections, highlighting the importance of combining conventional and complementary approaches, as appropriate.
1. Efficacy verification
Efficacy verification, concerning botanical treatments for Human Papillomavirus infections, centers on demonstrating that a specific herbal intervention produces measurable and clinically relevant results. A causal relationship must be established, wherein the administration of the herbal remedy demonstrably leads to a reduction in viral load, clearance of lesions, or improvement in associated symptoms. Its importance stems from the imperative to distinguish between anecdotal evidence and scientifically validated therapeutic effects.
The absence of robust efficacy verification leaves individuals vulnerable to ineffective treatments, potentially delaying or forgoing conventional medical interventions that have established efficacy. For example, numerous herbal products are marketed with claims of antiviral properties, yet few have undergone rigorous clinical trials specifically targeting HPV. In cases where studies exist, methodological flaws, such as small sample sizes or lack of control groups, often limit the conclusions. The practical significance of establishing efficacy lies in providing healthcare providers and patients with reliable information upon which to base informed treatment decisions.
In summary, efficacy verification for botanical approaches in managing HPV is essential for patient safety and responsible healthcare practices. Challenges remain in conducting methodologically sound research in this area, and continued efforts are needed to rigorously evaluate the true potential of herbal interventions. A focus on stringent scientific standards and transparent reporting of results is crucial for advancing the field and ensuring that patients receive effective and evidence-based care.
2. Safety Profiles
The determination of safety profiles is paramount when considering plant-derived interventions for Human Papillomavirus infections. A comprehensive safety profile encompasses the assessment of potential adverse effects, contraindications, and interactions associated with the herbal remedy. It is causally linked to responsible healthcare practices, ensuring that the potential benefits outweigh the risks. Without adequate understanding of safety implications, individuals may experience unintended and detrimental health consequences. For example, some herbs marketed for immune enhancement may interact with immunosuppressant medications, posing a significant risk to patients undergoing organ transplantation or autoimmune disease management.
The composition of herbal products can vary considerably based on factors such as plant origin, cultivation methods, and extraction processes. This variability directly impacts the consistency of the safety profile. Consequently, rigorous quality control measures and standardized manufacturing practices are essential. An example is the case of Aristolochia species, certain of which contain nephrotoxic compounds, but have been inadvertently included in herbal preparations. Clear labeling and disclosure of ingredients are fundamental to ensuring informed consumer choice. The practical application of this knowledge translates to clinicians and patients being equipped to assess the suitability of a given herbal treatment in light of individual health conditions and concurrent medications.
In summary, the safety profile represents a critical component of evaluating plant-based approaches to HPV management. It is not merely an ancillary consideration, but rather an integral element that dictates the ethical and responsible use of herbal interventions. The challenge lies in establishing robust safety data through well-designed clinical trials and post-market surveillance programs. Future progress necessitates a collaborative effort among researchers, healthcare professionals, and regulatory bodies to foster a culture of safety and evidence-based practice in the realm of plant-derived remedies.
3. Dosage standardization
Dosage standardization constitutes a crucial element in the responsible application of botanical interventions for Human Papillomavirus infections. Inherent variability in herbal product composition necessitates precise dosage control to achieve consistent therapeutic effects and minimize potential adverse reactions.
- Active Compound Quantification
Herbal remedies comprise a complex mixture of chemical constituents. Dosage standardization requires identifying the active compound(s) responsible for the purported antiviral or immunomodulatory effects. Accurate quantification of these compounds in each batch of product is essential. For instance, if an herbal extract claims to contain a specific concentration of curcumin, laboratory testing must confirm the accuracy of that claim. Failure to quantify active compounds introduces uncertainty and increases the risk of either subtherapeutic effects or toxicity.
- Bioavailability Considerations
Bioavailability refers to the extent and rate at which an active compound is absorbed into the bloodstream and becomes available at the target site. Dosage standardization must account for bioavailability. Certain herbal constituents exhibit poor bioavailability, requiring higher dosages or specific formulations to enhance absorption. Piperine, found in black pepper, is known to enhance the bioavailability of curcumin. Neglecting bioavailability considerations can lead to ineffective treatments, even with accurate quantification of active compounds.
- Patient-Specific Factors
Dosage standardization must consider individual patient characteristics, such as age, weight, renal function, and liver function. These factors influence drug metabolism and clearance, potentially altering the effective dosage. For example, patients with impaired liver function may require lower dosages to avoid accumulation of active compounds and potential hepatotoxicity. A one-size-fits-all approach to dosage is inappropriate and can increase the risk of adverse events.
- Standardized Extracts vs. Whole Herbs
Dosage standardization is generally easier to achieve with standardized extracts, which contain a known concentration of the active compound(s). Whole herbs, on the other hand, contain a complex mixture of constituents, making dosage standardization more challenging. While some proponents argue that whole herbs offer synergistic benefits, the lack of precise dosage control increases the risk of variability and inconsistent therapeutic effects. The choice between standardized extracts and whole herbs should be guided by scientific evidence and clinical judgment.
In conclusion, accurate dosage standardization is indispensable for the safe and effective use of botanical remedies in the context of Human Papillomavirus infections. It addresses the variability in herbal product composition, bioavailability considerations, patient-specific factors, and the choice between standardized extracts and whole herbs. Without dosage standardization, the potential benefits of herbal interventions remain uncertain, and the risk of adverse events increases substantially. Future research should prioritize the development of standardized herbal products and the establishment of evidence-based dosage guidelines.
4. Herbal interactions
The phenomenon of “herbal interactions” holds critical relevance within the context of “hpv herbal cures”. It addresses the potential for botanical remedies to interact with conventional pharmaceuticals, other herbal supplements, or even dietary components, altering their respective effects. This interaction can either enhance or diminish the therapeutic benefits of each substance or, more concerningly, lead to adverse reactions.
- Pharmacokinetic Interactions
Pharmacokinetic interactions pertain to alterations in the absorption, distribution, metabolism, and excretion (ADME) of a drug or herb due to the presence of another substance. For example, St. John’s Wort, often used for mood regulation, can induce the CYP3A4 enzyme, which metabolizes many conventional antiviral medications. Consequently, concurrent use may reduce the effectiveness of antiviral drugs used to manage HPV. Conversely, grapefruit juice, while not an herb, inhibits CYP3A4, potentially increasing drug concentrations and leading to toxicity. In the context of “hpv herbal cures,” it is crucial to assess whether specific herbs interfere with the metabolism of any conventional antiviral or immunomodulatory therapies.
- Pharmacodynamic Interactions
Pharmacodynamic interactions involve synergistic or antagonistic effects at the receptor or cellular level. For example, both an herbal remedy and a pharmaceutical drug might bind to the same receptor, either enhancing or blocking each other’s action. An illustrative case is the combined use of blood-thinning herbs, such as ginger or ginkgo, with anticoagulant drugs like warfarin. The synergistic effect increases the risk of bleeding. When considering “hpv herbal cures,” it is important to evaluate whether any herbs possess similar mechanisms of action as conventional treatments, potentially leading to additive effects or counteracting each other.
- Herb-Drug Interactions Affecting Immunomodulation
Some botanical remedies are promoted for their immunomodulatory properties, aiming to enhance the body’s natural defenses against HPV. However, certain herbs can interact with immunosuppressant drugs, which are used to prevent organ rejection or manage autoimmune diseases. For instance, Echinacea, often used to stimulate the immune system, may interfere with the efficacy of immunosuppressants, increasing the risk of organ rejection in transplant recipients. When integrating “hpv herbal cures,” caution must be exercised to ensure that the herbs do not antagonize or exacerbate the effects of any immunosuppressive medications the patient is taking.
- Impact on Diagnostic Testing
Certain herbs can interfere with laboratory tests used to monitor the progression of HPV infection or assess the efficacy of treatments. For example, some herbal supplements can affect liver enzyme levels, potentially complicating the interpretation of liver function tests. If an individual is undergoing “hpv herbal cures” and also receiving conventional medical care, it is imperative to inform the healthcare provider about all herbs being taken to ensure accurate interpretation of diagnostic results. Failure to do so can lead to misdiagnosis or inappropriate treatment adjustments.
These facets underscore the imperative for careful consideration of herbal interactions when exploring botanical remedies for HPV. Healthcare providers need to conduct thorough medication reconciliation, documenting all herbal supplements a patient is taking, to identify potential interactions and minimize the risk of adverse events. The interplay between conventional medicine and complementary therapies requires a nuanced approach, emphasizing patient safety and evidence-based decision-making.
5. Immune modulation
Immune modulation represents a central tenet within the framework of botanical interventions for Human Papillomavirus infections. The body’s immune system serves as the primary defense against HPV, and its ability to recognize and eliminate the virus directly influences the course of infection. Thus, herbal remedies purported to influence immune function are often considered in conjunction with, or as alternatives to, conventional medical treatments. This approach operates on the premise that enhancing immune competence can facilitate viral clearance and prevent the progression of HPV-related conditions, such as cervical dysplasia. For example, certain polysaccharides derived from medicinal mushrooms, like Ganoderma lucidum (Reishi), are hypothesized to stimulate immune cell activity, potentially enhancing the body’s ability to combat HPV.
The connection between immune modulation and HPV management is complex and not fully elucidated. While some herbal constituents exhibit in vitro and in vivo immunomodulatory effects, translating these findings into clinically significant outcomes remains challenging. The precise mechanisms by which herbal remedies interact with the immune system are often unclear, and the effects can vary depending on factors such as individual immune status, dosage, and duration of treatment. Furthermore, the definition of “immune modulation” itself can be broad, encompassing a range of effects from stimulating immune cell proliferation to suppressing inflammatory responses. The practical significance of understanding this connection lies in the potential to develop more targeted and effective immunomodulatory strategies for HPV management. However, caution is warranted, as indiscriminate immune stimulation can potentially exacerbate autoimmune conditions.
In summary, the concept of immune modulation forms a cornerstone of the rationale behind employing botanical interventions for HPV. However, the efficacy and safety of these approaches require rigorous scientific evaluation. The current understanding of the complex interplay between herbal remedies and the immune system is incomplete, necessitating continued research to identify promising compounds, elucidate their mechanisms of action, and establish evidence-based guidelines for their use. Until more definitive data are available, a cautious and informed approach, guided by healthcare professionals, is essential when considering herbal remedies for immune modulation in the context of HPV.
6. Product sourcing
The origin and procurement of botanical materials significantly impact the safety and efficacy of purported “hpv herbal cures.” Sourcing practices directly influence product quality, constituent consistency, and the potential for contamination, thereby affecting therapeutic outcomes.
- Geographic Origin and Environmental Factors
The environment in which plants are grown affects their chemical composition. Soil quality, climate, and altitude can alter the concentration of active compounds and the presence of contaminants such as heavy metals or pesticides. For instance, herbs sourced from polluted areas may contain toxins that negate any potential therapeutic benefits. Selecting suppliers who prioritize sustainable and ethical harvesting practices, with verifiable quality control measures, is essential.
- Cultivation and Harvesting Methods
Cultivation techniques, including the use of fertilizers and pesticides, directly impact the purity of the final product. Wildcrafting, while seemingly natural, can lead to overharvesting and species endangerment. Moreover, improper harvesting methods can introduce contaminants. For instance, if roots are not properly cleaned after harvesting, soil-borne pathogens may persist. Suppliers who employ Good Agricultural and Collection Practices (GACP) are more likely to provide high-quality and safe herbal materials.
- Processing and Manufacturing Procedures
The methods used to process and manufacture herbal products, such as drying, extraction, and encapsulation, influence their potency and bioavailability. Inadequate drying can lead to mold growth, while inappropriate extraction techniques can degrade active compounds. Similarly, substandard manufacturing practices can result in contamination with adulterants or incorrect dosages. Reputable manufacturers adhere to Good Manufacturing Practices (GMP) to ensure product consistency and purity.
- Authentication and Quality Control
Adulteration and misidentification are prevalent issues in the herbal industry. Products labeled as one species may, in fact, contain a different species or even be entirely synthetic. Authentication through macroscopic and microscopic examination, as well as chemical fingerprinting, is necessary to ensure the correct species is used. Quality control measures, such as testing for heavy metals, pesticides, and microbial contamination, are essential to guarantee product safety. Certificates of Analysis (COAs) from independent laboratories provide valuable documentation of product quality.
The integration of verified product sourcing practices is paramount for mitigating risks associated with “hpv herbal cures.” Clinicians and patients alike must prioritize products from suppliers who demonstrate a commitment to quality, sustainability, and ethical sourcing. The potential for harm from contaminated or misidentified herbal products underscores the need for rigorous scrutiny of sourcing practices within the complementary and alternative medicine landscape.
7. Medical oversight
The application of botanical remedies for Human Papillomavirus infections necessitates stringent medical oversight to ensure patient safety and optimize treatment outcomes. A direct correlation exists between the level of medical supervision and the potential for adverse events or therapeutic failures. Self-treatment with herbal products, without proper diagnosis and monitoring, can delay or preclude effective conventional medical interventions. For example, a persistent HPV infection may progress to cervical dysplasia or cancer if reliance is placed solely on unproven herbal remedies, while neglecting recommended screening and treatment protocols. The importance of medical oversight lies in its capacity to integrate botanical approaches into a comprehensive management plan, tailoring treatment to individual patient needs and disease characteristics.
Medical oversight encompasses several critical components. Initial diagnostic evaluation, including Pap smears and HPV testing, establishes a baseline understanding of the infection. Regular monitoring allows for the assessment of treatment response and the detection of any adverse effects. Furthermore, medical professionals can identify potential interactions between herbal remedies and conventional medications, minimizing the risk of harmful outcomes. A practical example involves a patient taking an herbal supplement purported to boost immune function. Without medical oversight, the potential interaction of this supplement with other medications, such as immunosuppressants or antiviral drugs, may be overlooked, potentially leading to adverse consequences. Integration with evidence-based medical therapies is paramount.
In conclusion, medical oversight is not merely an ancillary consideration but rather an indispensable element in the responsible use of botanical remedies for HPV. It facilitates informed decision-making, promotes patient safety, and ensures that herbal approaches are integrated appropriately into a comprehensive management strategy. The absence of medical supervision can lead to delayed diagnosis, ineffective treatment, and potential adverse events. Continued research and education are needed to enhance healthcare professionals’ understanding of herbal interactions and to establish evidence-based guidelines for the safe and effective integration of botanical remedies into HPV management.
Frequently Asked Questions Regarding Botanical Interventions for HPV
The following section addresses common inquiries related to the utilization of plant-based remedies in the management of Human Papillomavirus infections. These answers aim to provide clear, evidence-based information to aid informed decision-making.
Question 1: Are herbal cures for HPV scientifically proven?
The assertion that herbal remedies definitively “cure” HPV lacks robust scientific validation. While some botanical compounds exhibit in vitro antiviral activity, clinical trials demonstrating consistent and significant efficacy in clearing HPV infections in vivo are limited. Further research is warranted to establish the true therapeutic potential of herbal interventions.
Question 2: What are the potential risks associated with using herbal treatments for HPV?
Potential risks include allergic reactions, interactions with conventional medications, and the use of contaminated or adulterated products. Some herbs can also exhibit toxic effects when ingested in high doses or over prolonged periods. Medical consultation is essential to assess individual risk factors and ensure safe usage.
Question 3: Can herbal remedies replace conventional medical treatments for HPV?
Herbal remedies should not be considered a replacement for conventional medical treatments, such as Pap smears, colposcopy, and LEEP procedures, which are proven effective in detecting and managing HPV-related cervical abnormalities. Herbal interventions may be considered as complementary therapies under the guidance of a healthcare professional, but should not delay or substitute for standard medical care.
Question 4: How can one ensure the quality and safety of herbal products?
To ensure quality and safety, herbal products should be sourced from reputable suppliers who adhere to Good Manufacturing Practices (GMP) and provide Certificates of Analysis (COAs) verifying purity and potency. Thoroughly review product labels for ingredient lists and potential allergens. Consult with a healthcare provider or pharmacist for guidance on selecting appropriate and safe herbal products.
Question 5: What role does the immune system play in HPV management, and how do herbal remedies affect it?
The immune system plays a crucial role in clearing HPV infections. Certain herbal remedies are purported to enhance immune function, but the extent and mechanisms of this effect remain under investigation. A balanced diet, regular exercise, and stress management are also essential for maintaining a healthy immune system. Indiscriminate immune stimulation may be detrimental, especially for individuals with autoimmune conditions.
Question 6: Where can one find reliable information about herbal treatments for HPV?
Reliable information can be obtained from reputable sources such as peer-reviewed scientific journals, government health agencies (e.g., the National Institutes of Health), and qualified healthcare professionals. Be wary of unsubstantiated claims made on websites or in marketing materials. Critically evaluate the evidence and consult with a healthcare provider for personalized guidance.
These responses highlight the importance of approaching botanical interventions for HPV with caution and prioritizing evidence-based medical care. Consultation with a healthcare professional is crucial for informed decision-making and safe management of HPV infections.
The subsequent sections will explore alternative strategies for managing HPV infections, emphasizing the importance of preventative measures and early detection.
Conclusion
The discourse surrounding “hpv herbal cures” necessitates a discerning approach, tempered by scientific rigor and medical prudence. Exploration has revealed a landscape characterized by limited clinical validation, potential safety concerns, and the crucial need for informed decision-making. Reliance solely on unproven botanical remedies may delay or preclude effective conventional medical interventions, potentially jeopardizing patient health. The complex interplay between herbal constituents and the human immune system warrants continued investigation to elucidate their precise mechanisms of action and potential therapeutic benefits.
Prudent action dictates that individuals prioritize established medical protocols for HPV management, including regular screening, vaccination, and appropriate treatment of precancerous lesions. Complementary use of botanical remedies should only be considered under the guidance of qualified healthcare professionals, with careful consideration of potential interactions and individual patient circumstances. A future outlook mandates robust scientific research, standardized product manufacturing, and comprehensive medical oversight to ensure patient safety and to accurately assess the true potential of plant-derived interventions in addressing Human Papillomavirus infections.