The consumption of plant-derived infusions during gestation warrants careful consideration. Several factors, including the specific botanical composition and the physiological state of the individual, influence the safety profile. Potential effects range from benign hydration to adverse interactions with maternal or fetal health. The noun phrase “herbal tea” denotes a beverage prepared by steeping plant materials, distinct from true teas derived from the Camellia sinensis plant.
Selecting appropriate beverages during pregnancy is crucial for maintaining hydration and overall well-being. Traditionally, certain botanical preparations have been used for their purported health benefits. However, the physiological changes associated with gestation may alter the impact of these preparations. Understanding the potential risks and benefits associated with various plants is paramount for informed decision-making. The lack of rigorous scientific studies on many herbal preparations necessitates a cautious approach.
Subsequently, this discussion will delve into frequently asked questions regarding the ingestion of specific herbal infusions during pregnancy. Each botanical will be examined in terms of its known properties, potential risks, and current recommendations for use. This information is intended to provide a comprehensive overview, facilitating informed choices concerning maternal health and fetal development.
Considerations for Herbal Tea Consumption During Pregnancy
This section provides guidance on the judicious selection and use of herbal teas during gestation, emphasizing safety and informed decision-making.
Tip 1: Consult with a Healthcare Provider: Prior to incorporating any herbal tea into the diet, seek advice from a qualified healthcare professional. Obstetricians, midwives, and registered dietitians possess the expertise to evaluate individual circumstances and provide personalized recommendations.
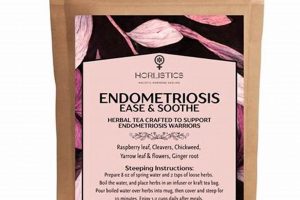
Tip 2: Identify the Specific Herbs: Determine the precise botanical composition of the tea. Many commercially available blends contain a mixture of herbs. A thorough understanding of each ingredient is essential for assessing potential risks and benefits.
Tip 3: Research Potential Contraindications: Investigate the known contraindications of each herb, particularly in relation to pregnancy. Certain herbs possess properties that may stimulate uterine contractions, elevate blood pressure, or interfere with medication absorption.
Tip 4: Monitor for Allergic Reactions: Be vigilant for any signs of an allergic reaction, such as skin rashes, itching, swelling, or difficulty breathing. Discontinue use immediately if any adverse symptoms arise and seek medical attention.
Tip 5: Practice Moderation: Even with generally considered safe herbs, moderation is crucial. Excessive consumption may lead to unforeseen complications. Adhere to recommended serving sizes and limit daily intake.
Tip 6: Choose Reputable Brands: Select herbal teas from reputable manufacturers that adhere to quality control standards. Look for products that are certified organic and free from contaminants, such as heavy metals and pesticides.
Tip 7: Be Aware of Potential Drug Interactions: Herbal teas can interact with prescription and over-the-counter medications. Disclose all medications and supplements to the healthcare provider to avoid adverse interactions.
Adherence to these guidelines promotes the safe and responsible use of herbal teas during pregnancy, minimizing potential risks to both maternal and fetal well-being.
The following sections will explore specific herbal teas commonly consumed during pregnancy, providing detailed information on their safety profiles and recommended usage.
1. Specific Herb Identification
The accurate determination of herbal components within any tea intended for consumption during pregnancy is of paramount importance. Misidentification or incomplete knowledge of the botanical constituents can lead to unintended and potentially harmful consequences for both the expectant mother and the developing fetus.
- Latin Nomenclature and Standardization
Utilizing the correct Latin botanical name ensures precise identification. Common names vary regionally and can refer to different plants with differing properties. Standardization, where available, guarantees a consistent concentration of active compounds, aiding in accurate risk assessment. For example, mistaking Mentha pulegium (pennyroyal), which is unsafe during pregnancy, for Mentha spicata (spearmint), which is generally considered safe in moderation, poses a significant hazard.
- Potential for Adulteration and Contamination
Commercial herbal tea products may be subject to adulteration with undeclared ingredients or contamination with heavy metals, pesticides, or bacteria. Independent laboratory testing and certification can mitigate these risks. Reliance solely on product labeling may be insufficient, particularly with less reputable brands. The presence of undeclared herbs known to be uterotonic (stimulating uterine contractions) poses a direct threat to pregnancy.
- Bioactive Compound Variability
The concentration of bioactive compounds within a given herb can vary significantly depending on factors such as growing conditions, harvesting methods, and processing techniques. This variability makes it challenging to predict the effects of a given tea on the body. Therefore, even if an herb is generally considered safe, variations in its chemical composition could lead to unexpected reactions. For instance, the level of pyrrolizidine alkaloids (PAs) in comfrey, a known hepatotoxin, can vary significantly, making it difficult to determine a safe dosage.
- Potential for Synergistic or Antagonistic Effects
Herbal tea blends often contain multiple ingredients, and the interaction of these ingredients can produce synergistic or antagonistic effects that are not fully understood. A combination of herbs that are individually considered safe may, in combination, exert undesirable effects. Further research is needed to fully elucidate these complex interactions and inform safe usage guidelines during pregnancy. The simultaneous consumption of herbs with hypotensive (blood pressure lowering) effects could, for example, lead to dangerously low blood pressure in susceptible individuals.
Therefore, the process of determining whether consumption is safe necessitates a rigorous evaluation of the ingredients and their potential effects, emphasizing the critical importance of verifying the specific herbs present and consulting with healthcare professionals prior to their use. The potential synergistic or antagonistic effects among herbs can dramatically shift the landscape from one deemed safe to one that presents significant risk.
2. Potential Maternal Risks
The consideration of potential maternal risks is central to any assessment of whether to ingest botanical infusions during pregnancy. These risks encompass a spectrum of adverse effects ranging from mild discomfort to severe complications, directly impacting maternal health and, consequently, fetal well-being. Careful evaluation of these risks is vital for informed decision-making.
- Uterine Contractions and Miscarriage
Certain herbal constituents possess uterotonic properties, capable of stimulating uterine contractions. In early pregnancy, this may increase the risk of miscarriage. In later stages, premature labor could be induced. Herbs such as blue cohosh and pennyroyal are known to carry this risk. Determining whether an herbal tea contains such constituents is crucial. This factor underscores the necessity for detailed ingredient scrutiny and consultation with healthcare professionals.
- Changes in Blood Pressure
Some herbs can significantly alter maternal blood pressure. Elevation of blood pressure can exacerbate pre-existing hypertension or induce pre-eclampsia, a serious pregnancy complication. Conversely, a drastic decrease in blood pressure may compromise placental perfusion, jeopardizing fetal oxygenation. Licorice root, for example, is known to elevate blood pressure. Monitoring for potential hypertensive or hypotensive effects is imperative.
- Interference with Medication
Herbal constituents can interact with prescription or over-the-counter medications, altering their efficacy or increasing the risk of adverse effects. This is particularly relevant for pregnant individuals managing pre-existing conditions or requiring medications for pregnancy-related complications. St. John’s Wort, for example, can affect the metabolism of various medications. Disclosure of all herbal tea consumption to healthcare providers is essential to avoid potential drug interactions.
- Gastrointestinal Distress
Certain herbs can cause gastrointestinal disturbances such as nausea, vomiting, diarrhea, or abdominal cramping. While these symptoms may be relatively mild in some individuals, they can contribute to dehydration and electrolyte imbalances, which are particularly concerning during pregnancy. Peppermint, while often used to alleviate nausea, can exacerbate heartburn in some individuals. Awareness of potential gastrointestinal side effects is important for informed selection of herbal teas.
The potential for maternal risks dictates that any decision regarding herbal tea ingestion be approached with caution. These risks highlight the necessity for rigorous evaluation of each herb’s properties, careful monitoring for adverse effects, and open communication with healthcare providers. A thorough understanding of these risks is crucial for promoting maternal and fetal well-being.
3. Fetal Development Impact
The influence on fetal development is a primary consideration when evaluating the safety of consuming botanical infusions during gestation. The developing fetus is particularly vulnerable to exogenous substances, as organogenesis and rapid cellular differentiation occur throughout pregnancy. Exposure to certain compounds present in herbal teas can disrupt these critical processes, leading to a range of adverse outcomes. The timing and duration of exposure, as well as the specific compounds involved, are key determinants of the severity of the impact. The direct link between maternal ingestion and potential harm to the developing fetus underscores the importance of evidence-based decision-making. For example, consumption of teas containing high levels of pyrrolizidine alkaloids (PAs) has been linked to liver damage in newborns, demonstrating a direct toxic effect transmitted through the placenta. Another significant risk factor is the potential for endocrine disruption, where compounds mimic or interfere with natural hormones essential for fetal growth and development.
Specific examples further illustrate the potential for fetal harm. Certain herbs, due to their emmenagogue properties (stimulating menstruation), can induce uterine contractions, potentially leading to premature birth or miscarriage, particularly during the first trimester. Other herbs may contain compounds that cross the placental barrier and directly affect fetal organ systems. For instance, some botanical constituents have been associated with cardiac abnormalities or neural tube defects in animal studies. While human data may be limited for many herbal preparations, the precautionary principle dictates a conservative approach, particularly in the absence of robust safety data. The lack of standardized testing and regulation of herbal products further compounds the challenge of assessing fetal risk. Accurate labeling and transparent sourcing are crucial, but often lacking, requiring careful scrutiny and professional guidance.
In conclusion, the potential for fetal development impact necessitates a cautious approach to herbal tea consumption during pregnancy. Understanding the specific constituents of herbal teas, their potential mechanisms of action, and the limitations of available safety data is crucial. The absence of definitive evidence of harm does not equate to safety; therefore, consultation with a qualified healthcare provider is essential to weigh the potential risks and benefits for each individual case. Prioritizing fetal well-being requires informed decision-making based on the best available evidence and a conservative approach to herbal supplementation.
4. Dosage Considerations
The relationship between dosage and safety during gestation is paramount when considering the consumption of herbal teas. While some botanical infusions may be deemed generally safe in small quantities, exceeding established limits can introduce significant risks for both the pregnant individual and the developing fetus. The impact is directly proportional to the concentration of bioactive compounds ingested, necessitating meticulous attention to recommended serving sizes and frequency of consumption. For example, chamomile tea, often considered a mild relaxant, may pose minimal risk when consumed in one or two cups daily. However, excessive intake could lead to increased drowsiness or, theoretically, exert mild blood-thinning effects. The precise threshold at which benefits outweigh risks remains individualized and requires professional medical guidance.
The variable potency of herbal preparations further complicates dosage determination. Factors such as growing conditions, harvesting methods, and processing techniques can significantly influence the concentration of active constituents in a given product. This variability underscores the importance of selecting reputable brands that adhere to stringent quality control standards. Moreover, the concurrent use of other herbal supplements or medications can amplify or diminish the effects of the herbal tea, necessitating a holistic assessment of potential interactions. For instance, combining an herbal tea with anticoagulant properties with a prescription blood thinner could elevate the risk of bleeding. Conversely, an herb with diuretic effects could exacerbate dehydration if taken alongside diuretic medication. Understanding the potential for additive or synergistic effects is crucial for informed decision-making.
In conclusion, careful consideration of dosage is an indispensable component of assessing the suitability of herbal tea consumption during pregnancy. The establishment of safe upper limits requires a comprehensive understanding of the specific botanical composition, the individual’s medical history, and the potential for interactions with other substances. Given the inherent uncertainties associated with herbal preparations, adherence to conservative dosage guidelines and proactive consultation with healthcare providers are essential for minimizing risks and promoting maternal and fetal well-being. The prudent approach entails prioritizing caution and evidence-based recommendations over anecdotal claims.
5. Preparation Methods
The methodology employed in preparing herbal infusions significantly impacts their safety and suitability during gestation. Variations in preparation techniques influence the concentration of bioactive compounds extracted from the plant material, thereby altering the potential for both beneficial and adverse effects. Precise control over preparation parameters is crucial for mitigating risks and maximizing the likelihood of a safe outcome.
- Steeping Time and Temperature
Prolonged steeping times and elevated water temperatures can extract higher concentrations of active constituents, potentially increasing the risk of adverse effects. Conversely, insufficient steeping may result in a weak infusion, rendering any potential therapeutic benefits negligible. The optimal steeping time and temperature vary depending on the specific herb and the desired concentration of bioactive compounds. A standardized approach, adhering to established guidelines, is essential. For instance, exceeding the recommended steeping time for certain herbs can release compounds that may stimulate uterine contractions.
- Herb-to-Water Ratio
The ratio of plant material to water directly affects the potency of the infusion. Using an excessive amount of herb can lead to an over-concentrated beverage with increased risk of adverse effects. Conversely, an insufficient amount of herb may result in a weak and ineffective infusion. Precise measurement of both the herb and the water is necessary to ensure consistency and safety. The use of standardized measuring tools, such as measuring spoons and cups, is recommended. Deviating from established ratios, particularly with potent herbs, can compromise maternal and fetal well-being.
- Filtration and Straining
Proper filtration and straining techniques remove particulate matter from the infusion, reducing the risk of gastrointestinal irritation and improving the palatability of the beverage. Failure to adequately filter or strain the infusion may result in the ingestion of unwanted plant debris, potentially leading to digestive discomfort. The use of fine-mesh strainers or tea filters is recommended to ensure a clear and smooth infusion. Removing particulate matter is particularly important for individuals with sensitive digestive systems.
- Source Water Quality
The quality of the water used to prepare herbal infusions can significantly impact their safety. Contaminated water may introduce harmful substances into the beverage, posing risks to both the pregnant individual and the developing fetus. The use of filtered or purified water is recommended to minimize the risk of contamination. Water sources should be free from heavy metals, bacteria, and other pollutants. Adherence to established water quality standards is essential for safe herbal tea preparation.
The careful control and standardization of preparation methods are crucial for ensuring the safety of herbal tea consumption during pregnancy. Precise measurement of ingredients, adherence to recommended steeping times and temperatures, and the use of high-quality water are all essential components of a safe and responsible approach. Neglecting these considerations can significantly increase the risk of adverse effects, underscoring the importance of informed decision-making and adherence to established guidelines.
6. Professional Consultation
The determination of whether the consumption of herbal teas is appropriate during gestation necessitates the involvement of qualified healthcare professionals. The complexity surrounding the physiological effects of various botanicals demands expertise in maternal health, pharmacology, and potential herb-drug interactions. Professional consultation serves as a cornerstone for informed decision-making, mitigating risks, and promoting optimal outcomes for both the pregnant individual and the developing fetus.
- Individualized Risk Assessment
Healthcare providers conduct a comprehensive assessment of the individual’s medical history, current health status, and any pre-existing conditions. This evaluation identifies potential contraindications or heightened sensitivities to specific herbal constituents. For instance, individuals with a history of miscarriage or pre-eclampsia require particularly cautious consideration, as certain herbs may exacerbate these conditions. This personalized approach ensures that recommendations are tailored to the unique circumstances of each pregnancy.
- Evidence-Based Recommendations
Healthcare professionals rely on scientific evidence and established clinical guidelines to formulate recommendations regarding herbal tea consumption. While definitive human studies on the safety of many herbs during pregnancy are limited, available data from animal studies, traditional use patterns, and pharmacological properties inform the decision-making process. This evidence-based approach prioritizes safety and minimizes reliance on anecdotal claims or unsubstantiated beliefs. For example, recommendations regarding chamomile tea are often based on its known calming effects and generally recognized safety profile, but excessive consumption is still discouraged.
- Herb-Drug Interaction Evaluation
Healthcare providers assess the potential for interactions between herbal constituents and any prescription or over-the-counter medications the individual is currently taking. Herbal teas can alter the absorption, metabolism, or excretion of certain drugs, leading to decreased efficacy or increased risk of adverse effects. For instance, St. John’s Wort, although not typically recommended during pregnancy, can interact with antidepressants and other medications, potentially compromising their effectiveness. A thorough review of all medications and supplements is essential for preventing harmful interactions.
- Monitoring and Management of Adverse Effects
Healthcare professionals provide guidance on monitoring for potential adverse effects and managing any complications that may arise from herbal tea consumption. This includes educating individuals about potential warning signs, such as uterine contractions, changes in blood pressure, or allergic reactions. Prompt reporting of any concerning symptoms is crucial for timely intervention and prevention of serious consequences. The availability of ongoing support and monitoring ensures that any adverse effects are addressed promptly and effectively.
The integration of professional consultation into the decision-making process surrounding herbal tea consumption during pregnancy is indispensable for safeguarding maternal and fetal well-being. By providing individualized risk assessments, evidence-based recommendations, herb-drug interaction evaluations, and monitoring for adverse effects, healthcare professionals empower individuals to make informed choices and minimize potential risks. This collaborative approach ensures that the use of herbal teas is aligned with the specific needs and circumstances of each pregnancy, promoting optimal outcomes for both mother and child.
Frequently Asked Questions
This section addresses common inquiries regarding the suitability of specific botanical infusions during gestation. Information presented herein is intended to inform and should not substitute professional medical advice.
Question 1: Is all herbal tea safe during pregnancy?
No. The safety profile of herbal teas during pregnancy varies significantly depending on the specific botanical components. Certain herbs may pose risks to both the pregnant individual and the developing fetus.
Question 2: How does one determine if an herbal tea is safe during pregnancy?
Consulting with a healthcare provider is crucial. Furthermore, a thorough review of the tea’s ingredients, potential contraindications, and reliable scientific information is necessary.
Question 3: What are some examples of herbal teas generally considered unsafe during pregnancy?
Herbs like pennyroyal, blue cohosh, and those containing high levels of pyrrolizidine alkaloids are generally considered unsafe due to potential uterotonic or toxic effects.
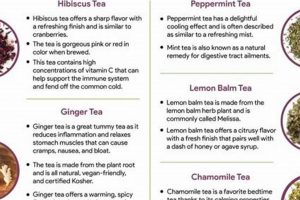
Question 4: Are there any herbal teas generally considered safe in moderation during pregnancy?
Chamomile, ginger, and peppermint teas are often considered safe in moderation, but this does not eliminate the need for professional medical advice prior to consumption.
Question 5: Can herbal teas interact with prescription medications during pregnancy?
Yes. Herbal constituents can interact with prescription medications, potentially altering their efficacy or increasing the risk of adverse effects. Disclosure of all herbal consumption to healthcare providers is essential.
Question 6: Is organic herbal tea inherently safer than non-organic?
Organic certification reduces the risk of pesticide exposure but does not guarantee safety. The inherent properties of the herb itself remain the primary safety consideration.
Therefore, the consumption of plant-derived infusions during gestation requires prudent evaluation and professional guidance. Self-medication with herbal teas during pregnancy is discouraged.
The subsequent section will offer a synthesis of key considerations regarding the safe and responsible use of herbal teas throughout gestation.
Can You Have Herbal Tea While Pregnant
The preceding exploration of “can you have herbal tea while pregnant” reveals the complexity inherent in evaluating the safety of botanical infusions during gestation. The identity of the herb, its potential effects on maternal and fetal physiology, appropriate dosage considerations, proper preparation methods, and the necessity for professional consultation emerge as critical factors. No blanket statement regarding safety is possible; each botanical must be assessed individually, considering the unique circumstances of the pregnancy.
Ultimately, responsible decision-making hinges on prioritizing evidence-based information and erring on the side of caution. Given the limitations of existing research and the potential for unforeseen consequences, consultation with a qualified healthcare provider is indispensable. The well-being of both mother and child demands a commitment to informed choices and a vigilant awareness of potential risks throughout gestation. Further research and standardized quality control measures within the herbal industry are vital to enhance the safety and transparency surrounding the consumption of herbal teas during this critical period.