Herbal infusions, carefully selected for their therapeutic properties, may offer a complementary approach to managing allergic reactions. These beverages, derived from various plants, aim to alleviate symptoms through natural compounds. For instance, certain herbs contain antihistamine or anti-inflammatory constituents, potentially reducing the body’s response to allergens.
The utilization of botanicals for health support possesses a rich historical precedent, with traditional medicinal systems worldwide incorporating herbal remedies for respiratory and immune-related ailments. Their perceived benefits include ease of access, relatively low cost, and a perceived gentler impact compared to some pharmaceutical interventions. However, it is crucial to acknowledge that efficacy and safety can vary depending on the specific herb, preparation method, and individual sensitivities.
The subsequent sections will delve into specific herbal options commonly considered for allergy symptom relief, examining their purported mechanisms of action and outlining important considerations regarding potential interactions, contraindications, and appropriate usage. The exploration focuses on presenting evidence-based information and promoting informed decision-making concerning the integration of these beverages into a holistic allergy management strategy.
Guidance on Selecting and Utilizing Beneficial Herbal Infusions
The following recommendations are designed to assist individuals in making informed choices regarding the incorporation of herbal beverages into an allergy management plan. Adherence to these suggestions may optimize potential benefits and minimize potential adverse effects.
Tip 1: Prioritize Consultation with a Healthcare Professional: Before initiating any new herbal regimen, engage in a discussion with a qualified healthcare provider. This step is crucial to ascertain the suitability of specific herbs, rule out potential interactions with existing medications, and address any pre-existing health conditions.
Tip 2: Emphasize Single-Ingredient Preparations Initially: When first exploring herbal infusions, commence with single-ingredient formulations. This approach facilitates the identification of potential sensitivities or adverse reactions to specific botanicals.
Tip 3: Source Reputable and Certified Products: Procure herbal teas from established and reputable suppliers. Look for certifications that indicate adherence to quality control standards, ensuring the purity and potency of the product. This minimizes the risk of contamination or adulteration.
Tip 4: Adhere to Recommended Dosage Guidelines: Strictly adhere to the dosage recommendations provided by the manufacturer or a qualified herbalist. Excessive consumption may increase the likelihood of adverse effects. Start with smaller quantities and gradually increase as tolerated.
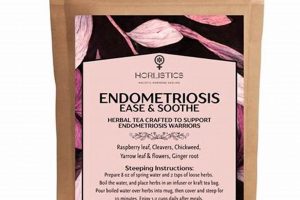
Tip 5: Prepare Infusions Correctly: Follow recommended brewing instructions. Optimal extraction of beneficial compounds depends on proper water temperature and steeping time. Deviations from prescribed methods may impact the tea’s efficacy.
Tip 6: Monitor for Allergic Reactions: Observe closely for any signs of allergic reaction, such as skin rashes, itching, swelling, or respiratory distress. Discontinue use immediately if any adverse symptoms develop and seek medical attention.
Tip 7: Be Mindful of Potential Interactions: Recognize that herbal constituents can interact with certain medications. Exercise particular caution if taking anticoagulants, immunosuppressants, or other prescription drugs. Consultation with a pharmacist or physician is strongly advised.
The application of these guidelines can facilitate a more informed and cautious approach to using herbal infusions as a supportive measure for managing allergy symptoms. Prioritizing safety and individual tolerance is paramount.
The article will now proceed to explore the potential benefits of various herbal infusions.
1. Plant compounds identified
The designation of an herbal infusion as optimal for allergy management relies heavily on the identification and characterization of its constituent plant compounds. The presence of specific compounds, possessing established antihistamine, anti-inflammatory, or mast-cell stabilizing properties, directly contributes to the potential efficacy of the herbal preparation. Without rigorous identification of these compounds, the rationale for using a particular herb for allergies remains speculative and lacks scientific grounding. For example, chamomile contains apigenin, a flavonoid with reported anti-inflammatory effects. The documented presence of apigenin in chamomile tea provides a plausible mechanism for its purported allergy-relieving properties.
The quantitative assessment of these plant compounds is also of critical importance. Variations in growing conditions, harvesting techniques, and processing methods can significantly influence the concentration of active constituents in the final product. Teas marketed with unsubstantiated claims, lacking analysis of their actual chemical composition, may offer negligible therapeutic benefit. Rigorous analytical methods, such as high-performance liquid chromatography (HPLC) or gas chromatography-mass spectrometry (GC-MS), are essential for verifying the presence and concentration of relevant compounds. The practical significance lies in ensuring that the consumer receives a product with a predictable and potentially beneficial level of activity.
In conclusion, the identification of plant compounds forms the bedrock upon which the concept of an ideal herbal infusion for allergy relief is built. This identification is not merely an academic exercise; it is a prerequisite for understanding the mechanism of action, predicting potential efficacy, and ensuring product quality. While anecdotal evidence may promote certain herbal remedies, a truly informed decision requires supporting data on the compounds present and their respective concentrations. Challenges remain in standardizing herbal preparations and ensuring consistent levels of active constituents, but the pursuit of rigorous chemical analysis remains crucial for advancing the field.
2. Antihistamine properties analyzed
The identification of herbal infusions as potentially suitable for allergy management hinges significantly on the objective analysis of their antihistamine properties. This assessment involves scrutinizing the ability of specific herbal constituents to counteract the effects of histamine, a key mediator in allergic reactions. Evaluating these properties is paramount to understanding the potential therapeutic value of the infusion.
- Histamine Receptor Blockade
Antihistamines function by blocking histamine receptors, specifically H1 receptors, located on various cells in the body. Analysis focuses on determining whether the herbal infusion contains compounds capable of effectively binding to these receptors, thereby preventing histamine from exerting its pro-inflammatory effects. This blockade reduces symptoms like itching, sneezing, and runny nose that are characteristic of allergic reactions. For example, if an herbal tea contains constituents that competitively bind to H1 receptors with an affinity comparable to established antihistamine medications, it may be considered a potentially useful tool for allergy symptom control. However, the effectiveness must be quantified through rigorous testing.
- Mast Cell Stabilization
Mast cells release histamine and other inflammatory mediators upon activation by allergens. Certain herbal compounds may possess the ability to stabilize mast cells, preventing or reducing the release of these substances. Analysis involves measuring the effect of the herbal infusion on mast cell degranulation in vitro or in vivo. If the tea can significantly inhibit the release of histamine and other mediators from mast cells, it suggests a mechanism by which it could alleviate allergy symptoms. Quercetin, found in some herbal infusions, has been investigated for its mast cell stabilizing properties.
- Quantification of Active Compounds
The presence of antihistamine compounds is insufficient; their concentration must be quantifiable. Effective analysis requires identifying the specific compounds responsible for antihistamine activity and measuring their concentration in the herbal infusion. Variations in growing conditions, processing methods, and storage can influence the levels of these compounds. If the analysis reveals only trace amounts of the active constituents, the infusion may not provide significant therapeutic benefit. Standardized extracts, with guaranteed levels of active compounds, are often preferred to ensure consistent efficacy.
- Bioavailability and Metabolism
The bioavailability of antihistamine compounds in the herbal infusion must be considered. Bioavailability refers to the extent to which these compounds are absorbed into the bloodstream and can reach their target tissues. Analysis involves studying the absorption, distribution, metabolism, and excretion (ADME) of the active constituents. Even if an herbal tea contains potent antihistamine compounds, they may be poorly absorbed or rapidly metabolized, limiting their therapeutic effect. Further research may be needed to optimize the delivery and bioavailability of these compounds.
The comprehensive analysis of antihistamine properties is critical in determining the suitability of any herbal infusion for allergy management. This analysis extends beyond mere identification of active compounds to include quantification, assessment of bioavailability, and characterization of their mechanisms of action. Thorough investigation is crucial for ensuring that these infusions are not only safe but also effectively contribute to managing allergy symptoms.
3. Inflammation reduction documented
The documented reduction of inflammation constitutes a pivotal factor in assessing the efficacy of an herbal infusion deemed potentially beneficial for allergy management. Allergic reactions are inherently linked to inflammatory processes, and any intervention aimed at alleviating symptoms must, at its core, address this underlying inflammation.
- Cytokine Modulation
Inflammation reduction is frequently mediated through the modulation of cytokine production. Certain herbal constituents may inhibit the release of pro-inflammatory cytokines, such as TNF-alpha and IL-6, while simultaneously promoting the production of anti-inflammatory cytokines like IL-10. Documented evidence of this activity, typically obtained through in vitro or in vivo studies, provides a rational basis for utilizing specific herbs to dampen the inflammatory response associated with allergies. The impact is significant as it directly affects the cascade of events leading to symptom exacerbation.
- Inhibition of Inflammatory Enzymes
Several enzymes, including cyclooxygenase (COX) and lipoxygenase (LOX), play a crucial role in the synthesis of inflammatory mediators, such as prostaglandins and leukotrienes. Herbal compounds that inhibit these enzymes can effectively reduce the production of these mediators, thereby alleviating inflammation. Documented evidence of such enzyme inhibition, supported by biochemical assays, strengthens the argument for the anti-inflammatory potential of a given herbal infusion. This mechanism offers a targeted approach to controlling inflammation at its source.
- Reduction of Oxidative Stress
Oxidative stress, characterized by an imbalance between the production of reactive oxygen species (ROS) and the capacity of the antioxidant defense system, contributes significantly to inflammation. Certain herbal compounds possess antioxidant properties, scavenging ROS and mitigating oxidative damage. Documented evidence demonstrating the ability of an herbal infusion to reduce oxidative stress provides additional support for its anti-inflammatory effects. This mechanism is particularly relevant in chronic inflammatory conditions associated with persistent allergies.
- Impact on Immune Cell Infiltration
Inflammation is often characterized by the infiltration of immune cells, such as neutrophils and eosinophils, into affected tissues. Herbal compounds that inhibit this infiltration can effectively reduce the inflammatory response. Documented evidence of reduced immune cell migration, observed through histological analysis or flow cytometry, indicates a significant impact on the inflammatory process. This aspect of inflammation reduction is critical in preventing tissue damage and promoting resolution of the inflammatory response.
The aggregation of evidence across these facets cytokine modulation, enzyme inhibition, oxidative stress reduction, and immune cell infiltration collectively informs the assessment of an herbal infusion’s anti-inflammatory potential. While anecdotal reports may suggest benefit, rigorous documentation of inflammation reduction, supported by scientific evidence, is essential for establishing a rational basis for the selection and utilization of the most effective herbal teas for allergy management. Lack of documented evidence necessitates caution, as it may indicate a lack of efficacy or potential harm.
4. Individual tolerance assessed
Determining the suitability of any herbal infusion, particularly in the context of allergy management, necessitates a rigorous assessment of individual tolerance. Variability in physiological responses dictates that no single herbal preparation universally qualifies as the “best” option. Adverse reactions, ranging from mild discomfort to severe hypersensitivity, may arise despite the inherent safety profile generally associated with herbal remedies.
- Genetic Predisposition
Genetic factors can significantly influence an individual’s response to specific herbal constituents. Variations in metabolic enzyme activity, such as cytochrome P450 enzymes, can alter the rate at which herbal compounds are processed and eliminated from the body. Individuals with reduced enzyme activity may experience prolonged exposure to active compounds, increasing the risk of adverse effects. Genetic testing, while not routinely performed, can provide insights into potential sensitivities or contraindications to specific herbs. In the absence of such testing, a cautious approach, involving incremental dose escalation and vigilant monitoring for adverse effects, is warranted.
- Pre-existing Conditions
The presence of pre-existing medical conditions can alter an individual’s tolerance to herbal infusions. Individuals with compromised liver or kidney function may exhibit reduced capacity to metabolize and excrete herbal constituents, leading to accumulation and potential toxicity. Similarly, individuals with gastrointestinal disorders may experience exacerbated symptoms, such as nausea, abdominal cramping, or diarrhea, following ingestion of certain herbs. A thorough medical history, obtained through consultation with a healthcare professional, is essential for identifying potential risks and tailoring the selection of herbal infusions accordingly.
- Allergic Sensitization
Prior exposure to a specific herb or botanically related species can lead to allergic sensitization. Subsequent exposure to the same herb may trigger an allergic reaction, ranging from mild skin rash to life-threatening anaphylaxis. Cross-reactivity, where an individual sensitized to one allergen develops a reaction to a structurally similar allergen, is also a consideration. For instance, individuals with ragweed allergies may exhibit cross-reactivity to chamomile or echinacea. Thorough evaluation of an individual’s allergy history is crucial for identifying potential cross-reactivity and avoiding herbal infusions that may provoke an allergic response. Skin prick testing or serum IgE testing can provide additional information regarding specific allergies.
- Drug Interactions
Herbal infusions can interact with conventional medications, altering their absorption, metabolism, or excretion. These interactions can lead to either decreased efficacy of the medication or increased risk of adverse effects. For example, St. John’s Wort, a common herbal remedy, can induce cytochrome P450 enzymes, accelerating the metabolism of numerous drugs, including oral contraceptives and immunosuppressants. Thorough review of an individual’s medication list, conducted by a pharmacist or physician, is essential for identifying potential drug interactions and adjusting dosages as necessary. In some cases, concurrent use of specific herbal infusions and medications may be contraindicated.
The confluence of these factors underscores the importance of individualizing the approach to herbal tea selection for allergy management. What proves beneficial for one individual may prove ineffective or even harmful to another. Consultation with qualified healthcare professionals, combined with careful self-monitoring, remains paramount in ensuring the safe and effective utilization of herbal infusions. The concept of a universally “best” tea is supplanted by the understanding that the ideal choice is contingent upon individual characteristics and circumstances.
5. Preparation methods optimized
The optimization of preparation methods constitutes a critical determinant in maximizing the therapeutic potential of herbal infusions for allergy management. Inadequate or inappropriate preparation can compromise the extraction of bioactive compounds, rendering the final beverage less effective or even inert. Consequently, meticulous attention to detail during preparation is essential to realize the intended benefits.
- Water Temperature Control
Water temperature profoundly affects the extraction of various phytochemicals. Excessive temperatures can degrade delicate compounds, such as volatile oils and certain flavonoids, reducing their therapeutic potency. Conversely, insufficient temperatures may fail to extract more robust compounds adequately. For most herbal teas, a water temperature between 200-212F (93-100C) is optimal, but delicate herbs like chamomile or green tea may benefit from slightly lower temperatures (around 170-185F or 77-85C) to preserve their beneficial properties. Thermometers should be used to ensure accurate temperature control.
- Steeping Time Adjustment
The duration of steeping directly influences the concentration of extracted compounds. Insufficient steeping results in a weak infusion with suboptimal levels of active constituents. Conversely, excessive steeping can release undesirable compounds, such as tannins, imparting a bitter taste and potentially negating some of the beneficial effects. General guidelines suggest steeping herbal teas for 5-10 minutes, but specific recommendations vary depending on the herb. For instance, roots and barks may require longer steeping times (10-20 minutes) to extract their compounds effectively.
- Herb to Water Ratio Calibration
The ratio of herb to water significantly impacts the potency of the infusion. An insufficient quantity of herb relative to water will yield a dilute beverage with limited therapeutic value. Conversely, an excessive quantity can lead to a concentrated infusion that may be unpalatable or even induce adverse effects. A general guideline is to use 1-2 teaspoons of dried herb per 8 ounces (240 ml) of water, but specific ratios may need to be adjusted based on the herb’s density and potency.
- Filtration and Storage Protocols
Proper filtration removes particulate matter that can affect the taste and texture of the tea. Fine-mesh strainers or unbleached tea filters are recommended to prevent the passage of small particles. Storage conditions also influence the stability of the infusion. Exposure to light, heat, and air can degrade sensitive compounds. It is best to consume freshly prepared tea immediately. If storage is necessary, the infusion should be kept in an airtight, opaque container in a cool, dark place for no more than 24 hours.
By meticulously adhering to optimized preparation methods, individuals can enhance the likelihood of realizing the intended benefits from herbal infusions for allergy management. Water temperature, steeping time, herb to water ratio, and storage methods must be carefully controlled to ensure the extraction, preservation, and stability of the active compounds. Failure to optimize these parameters can significantly diminish the therapeutic potential of even the most promising herbal remedies.
6. Symptom alleviation observed
The determination of an herbal tea’s status as potentially beneficial in allergy management culminates in the observation of actual symptom alleviation. While mechanistic studies and in vitro analyses provide valuable insights, the ultimate criterion rests upon demonstrable improvement in patient-reported outcomes. This section explores factors influencing the perception and interpretation of symptom alleviation within the context of herbal tea consumption.
- Subjective Reporting Bias
Symptom alleviation is, to a significant extent, a subjective experience. Patient-reported outcomes are susceptible to various biases, including the placebo effect, recall bias, and expectation bias. Individuals who anticipate benefit from an herbal tea may report improvements even in the absence of objective physiological changes. Conversely, individuals skeptical of herbal remedies may downplay or disregard any positive effects. Rigorous clinical trials, incorporating placebo controls and blinding procedures, are essential to minimize these biases and obtain more reliable assessments of symptom alleviation. The challenge lies in disentangling genuine therapeutic effects from psychological influences.
- Objective Measurement Challenges
Quantifying symptom alleviation in allergic conditions presents inherent challenges. Allergic symptoms, such as nasal congestion, sneezing, and itching, are often intermittent and variable in severity. Standardized scoring systems, such as visual analog scales or symptom diaries, can provide a more structured approach to symptom assessment, but these tools are still subject to individual interpretation. Objective measures, such as nasal lavage fluid analysis or pulmonary function tests, can supplement subjective reports, but they may not fully capture the totality of the patient’s experience. The integration of both subjective and objective measures is crucial for a comprehensive evaluation of symptom alleviation.
- Time Course of Symptom Relief
The time course of symptom relief can vary significantly depending on the herbal tea, the severity of the allergic reaction, and individual factors. Some individuals may experience rapid relief within hours of consuming the tea, while others may require days or weeks of consistent use before noticing any improvement. The delayed onset of action can be particularly challenging, as individuals may prematurely discontinue use before the herb has had sufficient time to exert its therapeutic effects. Realistic expectations regarding the time course of symptom relief are essential for promoting adherence to the treatment regimen. Furthermore, it is important to distinguish between acute relief of symptoms and long-term disease modification.
- Confounding Factors and Co-interventions
The observation of symptom alleviation can be confounded by numerous factors, including concurrent use of other medications, environmental exposures, and lifestyle modifications. Individuals who consume herbal tea for allergies may also be taking antihistamines, using nasal sprays, or avoiding known allergens. It can be difficult to isolate the specific contribution of the herbal tea to the observed symptom improvement. Careful consideration of these confounding factors, along with appropriate statistical adjustments, is essential for accurately assessing the efficacy of the herbal tea. In some cases, a washout period, during which all other allergy medications are discontinued, may be necessary to isolate the effects of the herbal tea.
In summary, while the observation of symptom alleviation is the ultimate goal in evaluating any potential remedy for allergies, a nuanced and critical approach is essential. Subjective biases, measurement challenges, variability in time course, and confounding factors must be carefully considered to avoid drawing premature or unsubstantiated conclusions. Rigorous clinical trials, incorporating appropriate controls and outcome measures, are necessary to definitively establish the efficacy of an herbal tea in alleviating allergy symptoms, ultimately contributing to its designation as a truly “best” choice.
Frequently Asked Questions
The following section addresses common inquiries regarding the use of herbal infusions as a complementary approach to managing allergy symptoms. These questions are intended to provide clarity and evidence-based information, fostering informed decision-making.
Question 1: What constitutes the “best herbal tea for allergies,” and is there a single universally effective option?
The notion of a single, universally “best” herbal infusion is misleading. Efficacy varies based on individual physiology, allergy triggers, and the specific composition of the herbal preparation. The most suitable option is determined through careful consideration of these factors and often necessitates a trial-and-error approach under professional guidance.
Question 2: How quickly can symptom relief be expected after initiating the consumption of herbal infusions?
The onset of symptom relief is highly variable. Some individuals may experience noticeable improvements within days, while others may require weeks of consistent consumption. This variability is influenced by the severity of the allergic reaction, the potency of the infusion, and individual metabolic factors. Patience and adherence to the recommended regimen are essential.
Question 3: Are herbal infusions a suitable replacement for conventional allergy medications, such as antihistamines or corticosteroids?
Herbal infusions are generally considered a complementary, rather than a replacement, therapy for conventional allergy medications. Individuals should not discontinue prescribed medications without consulting their healthcare provider. Herbal infusions may potentially reduce the reliance on pharmaceuticals in some cases, but this decision must be made in consultation with a medical professional.
Question 4: What are the potential risks and side effects associated with consuming herbal infusions for allergies?
Potential risks include allergic reactions to specific herbs, interactions with existing medications, and exacerbation of certain pre-existing conditions. Individuals with known allergies or medical conditions should exercise caution and consult with a healthcare provider before initiating herbal infusions. Adherence to recommended dosage guidelines is crucial to minimize the risk of adverse effects.
Question 5: How can the quality and safety of herbal tea products be ensured?
The quality and safety of herbal tea products can be enhanced by selecting reputable suppliers who adhere to Good Manufacturing Practices (GMP) and provide certificates of analysis (COAs) for their products. These certifications indicate that the products have undergone testing for purity, potency, and contaminants. Organic certification is also desirable to minimize exposure to pesticides.
Question 6: Can herbal infusions effectively address all types of allergies, including food allergies and severe anaphylactic reactions?
Herbal infusions are primarily intended for managing mild to moderate seasonal or environmental allergies. They are not a suitable treatment for food allergies or severe anaphylactic reactions. Individuals with food allergies or a history of anaphylaxis should always carry an epinephrine auto-injector and seek immediate medical attention in the event of an allergic reaction.
The information presented in this FAQ section is intended for educational purposes only and does not constitute medical advice. Consultation with a qualified healthcare professional is essential before initiating any new treatment regimen.
The subsequent sections will delve into practical considerations for integrating herbal infusions into a comprehensive allergy management plan.
Conclusion
This exploration has illuminated the multifaceted nature of selecting a purportedly “best herbal tea for allergies.” The designation is not absolute but contingent upon individual factors, including genetic predispositions, pre-existing conditions, and the specifics of the allergic response. While certain plant compounds within these infusions exhibit demonstrable antihistamine and anti-inflammatory properties, rigorous scientific validation remains imperative. Furthermore, optimal preparation methods and careful assessment of individual tolerance are paramount for maximizing potential benefits while mitigating risks.
Ultimately, the integration of herbal infusions into an allergy management strategy should be undertaken with informed awareness and professional guidance. Continued research is necessary to elucidate the precise mechanisms of action and establish standardized protocols for dosage and preparation. Until then, a cautious and individualized approach, prioritizing safety and evidenced-based decision-making, remains the most prudent course of action. Consultation with qualified healthcare professionals is strongly encouraged to ensure appropriate utilization and avoid potential adverse outcomes.