The confluence of traditional botanical remedies and gastroesophageal reflux disease presents a complex interaction. Certain plant-derived infusions are commonly consumed with the intent of alleviating digestive discomfort. However, the effects of these beverages on individuals experiencing acid reflux can vary significantly. For instance, while chamomile tea is often promoted for its calming properties, its impact on lower esophageal sphincter pressure is not universally beneficial.
The interest in using natural compounds to manage digestive ailments stems from a long history of herbal medicine practices across various cultures. Proponents highlight potential advantages such as reduced reliance on pharmaceutical interventions and the perceived gentleness of plant-based therapies. Nevertheless, the efficacy and safety of employing such methods in the context of chronic conditions require careful consideration. Scientific validation through rigorous clinical trials is essential to substantiate anecdotal claims and identify potential risks.
The following discussion will delve into specific herbal teas frequently used for gastrointestinal relief, examining their purported mechanisms of action and the existing evidence supporting or refuting their utility in managing acid reflux symptoms. Consideration will also be given to potential adverse reactions and interactions with conventional medications, emphasizing the need for informed decision-making in the use of these remedies.
Guidance on Herbal Infusions and Gastroesophageal Reflux Disease
The subsequent recommendations are intended to provide informed guidance on the selection and consumption of herbal infusions for individuals managing gastroesophageal reflux disease. These suggestions are for informational purposes and should not substitute professional medical advice.
Tip 1: Prioritize low-acidity herbal blends. Teas with inherently lower pH levels are less likely to exacerbate reflux symptoms. Options such as chamomile, licorice root (DGL form), and slippery elm are generally considered less acidic.
Tip 2: Consume herbal infusions between meals rather than immediately before or after. This spacing allows for more efficient digestion and reduces the likelihood of gastric distension contributing to reflux.
Tip 3: Moderate the temperature of the beverage. Excessively hot liquids can irritate the esophageal lining, potentially worsening reflux symptoms. Opt for lukewarm or slightly warm infusions.
Tip 4: Be mindful of added ingredients. Avoid adding citrus fruits, honey (in large quantities), or other acidic substances to herbal infusions, as these can counteract the intended benefits and trigger reflux episodes.
Tip 5: Monitor individual tolerance to specific herbs. Certain individuals may experience adverse reactions to specific botanicals. Maintain a record of consumed teas and any associated symptoms to identify potential triggers.
Tip 6: Consider the form of licorice root consumed. Deglycyrrhizinated licorice (DGL) is preferred, as it lacks the glycyrrhizin compound associated with potential blood pressure elevation. Standard licorice root should be avoided by individuals with hypertension.
Tip 7: Exercise caution with peppermint. While often touted for digestive relief, peppermint can relax the lower esophageal sphincter, potentially exacerbating acid reflux in susceptible individuals. Observe for adverse effects.
Adhering to these guidelines can assist in making more informed choices regarding the incorporation of herbal infusions into a reflux management strategy. Individual results may vary, and close monitoring of symptoms is paramount.
The following section will address potential contraindications and interactions between herbal remedies and conventional treatments for gastroesophageal reflux disease.
1. Symptom Exacerbation
Symptom exacerbation, in the context of herbal tea consumption and gastroesophageal reflux disease, denotes the worsening of existing reflux symptoms or the induction of new symptoms following the ingestion of specific herbal infusions. This phenomenon warrants careful investigation, as the intention behind consuming such teas is often to alleviate, rather than aggravate, digestive discomfort.
- Lower Esophageal Sphincter (LES) Relaxation
Certain herbal constituents can induce relaxation of the LES, the muscular valve preventing stomach acid from refluxing into the esophagus. Peppermint, for example, contains menthol, which is known to reduce LES pressure. This relaxation allows for easier backflow of gastric contents, thereby exacerbating heartburn and regurgitation.
- Acidity of Herbal Infusions
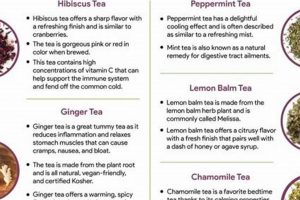
The pH level of an herbal tea can directly impact esophageal irritation. While many herbal teas are perceived as gentle, some may possess a sufficiently low pH to contribute to symptom exacerbation. Hibiscus tea, with its tart flavor profile, is an example of an herbal infusion that may exhibit a higher acidity level.
- Gastric Emptying Rate
Specific herbs can influence the rate at which the stomach empties its contents. Delayed gastric emptying prolongs the duration of gastric distension, increasing the pressure gradient favoring reflux. Certain herbal preparations might inadvertently slow down this process, leading to increased reflux episodes.
- Individual Sensitivities and Allergies
Individual responses to herbal substances can vary significantly. Undiagnosed sensitivities or allergies to specific herbs may manifest as gastrointestinal distress, mimicking or exacerbating GERD symptoms. Allergic reactions can trigger inflammation and increased sensitivity in the digestive tract, leading to heightened reflux perception.
These facets collectively underscore the importance of personalized assessment and cautious experimentation when incorporating herbal teas into a GERD management strategy. Recognizing the potential for symptom exacerbation necessitates careful selection of herbal infusions, mindful consumption practices, and diligent monitoring of individual responses. Understanding these factors will lead to more effective and safer use of herbal remedies.
2. Esophageal Sphincter Relaxation
The lower esophageal sphincter (LES) is a critical muscular valve situated at the junction of the esophagus and the stomach. Its primary function is to maintain unidirectional flow, allowing passage of ingested substances into the stomach while preventing the reflux of gastric contents back into the esophagus. Compromised LES function, characterized by relaxation or weakening, is a central pathophysiological mechanism in gastroesophageal reflux disease (GERD). This relaxation permits stomach acid to irritate the esophageal lining, leading to the hallmark symptoms of heartburn, regurgitation, and potential long-term complications such as esophagitis and Barrett’s esophagus.
Certain herbal teas contain compounds capable of influencing LES tone. Peppermint tea, for example, is known to contain menthol, a constituent demonstrated to relax smooth muscle, including the LES. This relaxation, while potentially beneficial for relieving other digestive issues, can inadvertently exacerbate GERD symptoms in susceptible individuals. Similarly, chamomile, though generally considered soothing, possesses compounds that may exert a mild relaxant effect on the LES in some individuals. The degree to which an herbal tea affects LES function varies based on factors such as the specific herbal constituents, concentration, individual physiology, and pre-existing LES competence. Therefore, caution is warranted when individuals with GERD consume herbal teas, particularly those known to influence smooth muscle tone.
The interplay between herbal tea consumption and LES function underscores the individualized nature of GERD management. While some individuals may tolerate certain herbal teas without adverse effects, others may experience symptom exacerbation due to LES relaxation. Empirically monitoring symptom responses and seeking guidance from healthcare professionals is essential for informed decision-making. The understanding of herbal teas impact on LES will help an individual make healthier decisions when it comes to choosing herbal remedies.
3. Acidity Levels Evaluated
The assessment of acidity levels in herbal teas is crucial in the context of gastroesophageal reflux disease (GERD). Gastric reflux involves the backflow of stomach acid into the esophagus, an event exacerbated by elevated acidity in the gastric contents. Certain herbal teas, despite their perceived mildness, may possess pH levels that contribute to, or worsen, reflux symptoms. Consequently, the evaluation of acidity in these beverages becomes a significant component in managing the interaction between herbal tea consumption and GERD.
For example, hibiscus tea, known for its tart flavor, often exhibits a lower pH compared to teas like chamomile or licorice root (DGL). The consumption of hibiscus tea by individuals with GERD may introduce additional acid into the digestive system, potentially triggering heartburn or regurgitation. Conversely, teas with a higher pH, or those that possess buffering capabilities, may be less likely to provoke such symptoms. Therefore, accurate measurement and consideration of acidity levels in herbal teas represent a practical step in mitigating the risk of exacerbating GERD.
In summary, the evaluation of acidity levels in herbal teas forms an essential aspect of understanding their potential impact on GERD. While not the sole determinant of a tea’s suitability for individuals with reflux, the acidity level serves as a critical factor to consider, alongside other characteristics such as potential effects on the lower esophageal sphincter. This evaluation, combined with individual tolerance monitoring, contributes to a more informed and personalized approach to managing GERD through dietary choices.
4. Herb-Drug Interactions
The concurrent use of herbal teas and pharmaceutical medications necessitates careful consideration due to the potential for herb-drug interactions. These interactions can alter the efficacy or toxicity of prescribed medications, impacting patient safety and therapeutic outcomes, particularly in the context of managing gastroesophageal reflux disease (GERD).
- Cytochrome P450 Enzyme Modulation
Many herbal constituents can modulate the activity of cytochrome P450 (CYP) enzymes, a family of hepatic enzymes responsible for metabolizing a wide range of drugs. Certain herbs may inhibit CYP enzymes, leading to increased drug concentrations and potential toxicity. Conversely, other herbs may induce CYP enzyme activity, resulting in decreased drug concentrations and reduced efficacy. For example, St. John’s Wort, while not typically consumed as a tea for GERD, is a potent CYP3A4 inducer and can significantly reduce the effectiveness of proton pump inhibitors (PPIs), a common medication for GERD.
- Pharmacodynamic Interactions
Pharmacodynamic interactions occur when herbs and drugs have additive, synergistic, or antagonistic effects on the same physiological system. For instance, licorice root (in its non-DGL form) possesses mineralocorticoid activity and can increase blood pressure. Concurrent use with antihypertensive medications may antagonize their effects, potentially leading to uncontrolled hypertension. In the context of GERD, an herb that relaxes the lower esophageal sphincter (LES) could counteract the effects of medications aimed at strengthening LES tone.
- Absorption Interference
Certain herbal components can interfere with the absorption of drugs in the gastrointestinal tract. This interference can occur through various mechanisms, including chelation, altered gastric pH, or effects on intestinal motility. For example, herbal teas containing tannins can bind to certain medications, reducing their absorption and bioavailability. Similarly, herbs that significantly alter gastric pH can affect the dissolution and absorption of pH-dependent drugs, such as certain antacids used for GERD relief.
- Potassium Depletion
Certain herbal teas, particularly those with diuretic properties, can lead to potassium depletion. Hypokalemia can potentiate the adverse effects of certain medications, such as digoxin, and may also exacerbate electrolyte imbalances in individuals taking diuretics for other medical conditions. While less directly related to GERD treatment, potassium depletion can indirectly impact overall health and complicate the management of GERD symptoms.
These interactions highlight the complex interplay between herbal teas and conventional medications used in the management of GERD. Individuals considering the use of herbal teas alongside prescription or over-the-counter medications should consult with a healthcare professional to assess potential risks and ensure safe and effective treatment. The assessment of herb-drug interactions are also very important when looking for herbal tea gerd effects.
5. Individual Tolerance Varies
Individual tolerance to herbal teas represents a critical factor in the context of gastroesophageal reflux disease (GERD). The physiological responses to specific herbal constituents can exhibit significant variability across individuals, influencing the occurrence and severity of reflux symptoms. This variability stems from differences in genetic predispositions, existing health conditions, medication use, and lifestyle factors, all of which can impact the digestive system’s sensitivity to herbal compounds. Consequently, an herbal tea deemed beneficial for one person may prove detrimental to another suffering from GERD.
For instance, chamomile tea is frequently cited for its calming properties and potential to ease digestive discomfort. However, while some individuals with GERD report symptom relief following chamomile consumption, others may experience increased heartburn or bloating. This discrepancy can be attributed to variations in gastric acid production, lower esophageal sphincter (LES) function, and individual sensitivities to compounds present in chamomile. Similarly, peppermint tea, often recommended for its antispasmodic effects, can exacerbate GERD symptoms in susceptible individuals due to its propensity to relax the LES. Recognizing and respecting individual tolerance is, therefore, essential in the safe and effective use of herbal teas for GERD management. A process of cautious experimentation and symptom monitoring can assist individuals in identifying herbal teas that are well-tolerated and provide relief, while avoiding those that trigger adverse reactions.
The practical significance of understanding individual tolerance lies in empowering individuals with GERD to make informed choices about their dietary and lifestyle habits. Rather than adhering to generalized recommendations, individuals are encouraged to adopt a personalized approach, carefully assessing their unique responses to various herbal teas. This approach necessitates meticulous record-keeping of consumed beverages, associated symptoms, and any other relevant factors, such as stress levels or concurrent medication use. By embracing a data-driven methodology, individuals can optimize their use of herbal teas for GERD management, minimizing the risk of adverse events and maximizing the potential for symptom relief.
Frequently Asked Questions
The following questions and answers address common inquiries regarding the relationship between herbal teas and gastroesophageal reflux disease (GERD). The information provided is intended for educational purposes and should not substitute professional medical advice.
Question 1: Is it universally safe for individuals with GERD to consume herbal teas?
No, the safety of herbal tea consumption for individuals with GERD is not universal. Specific herbal constituents can exacerbate reflux symptoms, such as heartburn and regurgitation, in certain individuals. Factors such as individual sensitivity, pre-existing conditions, and the specific composition of the herbal tea influence tolerance.
Question 2: Which herbal teas are generally considered less likely to trigger GERD symptoms?
Herbal teas such as chamomile, licorice root (in the deglycyrrhizinated, or DGL, form), and slippery elm are often cited as being less likely to trigger GERD symptoms. These teas are generally considered to have lower acidity and may possess soothing properties for the digestive tract. However, individual responses can vary.
Question 3: Can peppermint tea alleviate GERD symptoms?
Peppermint tea is often used for digestive complaints. However, the compounds in peppermint can relax the lower esophageal sphincter, potentially allowing stomach acid to flow back into the esophagus, which can worsen GERD symptoms. It is important to monitor any increase in symptoms when consuming peppermint tea.
Question 4: How does the acidity level of an herbal tea impact GERD symptoms?
The acidity level of an herbal tea can directly influence GERD symptoms. Teas with lower pH levels may irritate the esophageal lining, potentially exacerbating heartburn. Herbal teas with higher pH levels or buffering properties may be less likely to provoke such symptoms.
Question 5: Are there potential interactions between herbal teas and medications used to treat GERD?
Yes, potential interactions exist between herbal teas and medications used to treat GERD. Certain herbal constituents can alter the absorption, metabolism, or excretion of drugs, affecting their efficacy or toxicity. It is essential to consult a healthcare professional before combining herbal teas with prescription or over-the-counter medications.
Question 6: How can an individual determine their tolerance to specific herbal teas in the context of GERD?
Determining individual tolerance involves a process of cautious experimentation and symptom monitoring. A systematic approach includes tracking the consumption of specific herbal teas, documenting any associated symptoms, and consulting with a healthcare professional to assess potential risks and benefits.
In summary, the relationship between herbal teas and GERD is complex and multifaceted. Individual responses vary significantly, and careful consideration of factors such as herbal composition, acidity levels, potential interactions, and personal sensitivities is essential for safe and effective use.
The following section will explore lifestyle adjustments that can complement dietary modifications in managing GERD.
Conclusion
This exploration of the relationship between herbal tea and gastroesophageal reflux disease has revealed a multifaceted interaction. Key points include the variability in individual tolerance, potential for symptom exacerbation or mitigation, the significance of assessing acidity levels, and the imperative to consider herb-drug interactions. The information presented underscores that consumption of herbal teas is not a universally safe or beneficial practice for those managing GERD. Careful consideration of specific herbal properties and individual responses is paramount.
Given the complex and individualized nature of this interaction, it is essential to prioritize informed decision-making. Individuals with GERD considering the use of herbal teas should consult with healthcare professionals to assess potential risks and ensure safe and effective management of their condition. Further research is needed to fully elucidate the mechanisms by which various herbal constituents impact GERD and to establish evidence-based guidelines for their use.