The consumption of infusions derived from plants other than Camellia sinensis (true teas) during gestation is a common practice. These plant-based beverages are often perceived as natural and therefore safe. However, the physiological changes associated with pregnancy can alter how the body processes various substances, and the bioactive compounds in these infusions may exert different effects on both the mother and the developing fetus. For instance, chamomile infusions are sometimes used for relaxation, while ginger infusions are frequently consumed to alleviate nausea.
The perceived benefits of these botanical brews range from soothing digestive discomfort to promoting relaxation and improving sleep quality. Historically, various cultures have employed specific plants for medicinal purposes during pregnancy, passing down traditional knowledge through generations. While some plants have demonstrated potential therapeutic value, it’s crucial to acknowledge that not all botanical remedies are without risk. Regulation of herbal products often differs from that of pharmaceuticals, potentially leading to inconsistencies in product quality and concentration of active ingredients.
Given the potential for both benefits and risks, a comprehensive understanding of specific plants and their effects is paramount. This article will delve into considerations regarding the safety profiles of frequently consumed botanical infusions, emphasizing the importance of informed choices and consultation with healthcare professionals. Further discussion will include plants generally considered safe, those to avoid, and crucial factors in determining appropriate consumption during gestation.
Important Considerations Regarding Plant-Based Infusions During Gestation
Careful evaluation of safety and potential impacts is paramount when considering the incorporation of plant-based infusions into the diet during pregnancy. Informed decision-making, based on evidence-based information and professional guidance, is essential.
Tip 1: Conduct Thorough Research: Before consuming any plant-based infusion, investigate its known effects during pregnancy. Scientific literature and reputable sources can provide insight into potential risks and benefits.
Tip 2: Consult a Healthcare Provider: Open communication with a physician, midwife, or qualified herbalist is crucial. These professionals can assess individual risk factors, provide personalized recommendations, and consider potential interactions with existing medications or health conditions.
Tip 3: Exercise Moderation: Even if a plant-based infusion is generally considered safe, limiting intake is advisable. Excessive consumption may increase the risk of adverse effects.
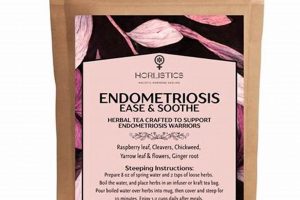
Tip 4: Source Products from Reputable Manufacturers: Choose plant-based infusions from trusted brands that adhere to quality control standards. This minimizes the risk of contamination and ensures accurate labeling of ingredients.
Tip 5: Be Aware of Potential Drug Interactions: Plant-based compounds can interact with pharmaceutical drugs. Inform healthcare providers of all herbal infusions consumed to prevent potential adverse interactions.
Tip 6: Monitor for Allergic Reactions: Individuals may experience allergic reactions to certain plants. Discontinue use immediately and seek medical attention if symptoms such as rash, itching, or difficulty breathing develop.
Tip 7: Avoid Infusions with Known Contraindications: Certain plants are recognized as unsafe during pregnancy due to potential teratogenic or abortifacient effects. It is imperative to avoid these infusions altogether.
Prudent consumption of plant-based infusions during pregnancy necessitates a balance between potential benefits and potential risks. Informed decision-making and professional guidance are key to safeguarding maternal and fetal well-being.
The subsequent sections will address specific plants commonly used in infusions, categorizing them according to their safety profiles during gestation.
1. Safety profiles
The safety profiles of botanical infusions during pregnancy represent a critical determinant in assessing their suitability for consumption. These profiles encompass a comprehensive understanding of the potential adverse effects, contraindications, and interactions associated with each specific plant. A lack of adequate safety data, particularly concerning teratogenicity or effects on fetal development, necessitates caution and may warrant complete avoidance. For example, infusions containing high concentrations of pyrrolizidine alkaloids, found in certain plants, are known to pose significant hepatotoxic and carcinogenic risks, making their use during pregnancy contraindicated.
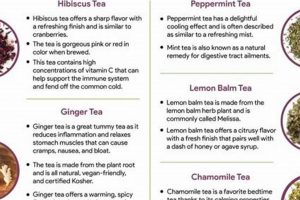
Understanding these profiles is crucial for informed decision-making. The absence of conclusive evidence of harm does not automatically equate to safety. Many botanical infusions lack rigorous clinical trials specifically assessing their effects on pregnant individuals. Therefore, reliance on traditional uses, anecdotal evidence, or extrapolations from non-pregnant populations may be insufficient. The practical significance of evaluating safety profiles lies in minimizing potential risks to both maternal and fetal health, preventing complications such as miscarriage, preterm labor, or developmental abnormalities. Infusions such as peppermint or chamomile, often considered safe in moderation, still require careful consideration due to individual sensitivities or potential interactions with existing medical conditions.
In summary, the examination of safety profiles forms the bedrock of responsible decision-making concerning the use of botanical infusions during gestation. Challenges arise from the limited availability of comprehensive research on specific herbs and the inherent variability in plant composition. By prioritizing evidence-based information, consulting with healthcare professionals, and exercising judicious caution, individuals can navigate the complexities of herbal infusion consumption during pregnancy and promote optimal outcomes.
2. Individual sensitivities
Individual sensitivities play a critical role in determining whether specific botanical infusions are appropriate during gestation. What might be considered a safe herbal infusion for one pregnant individual could elicit an adverse reaction in another due to variations in physiology, pre-existing conditions, or genetic predispositions. For instance, an individual with a known allergy to ragweed may experience cross-reactivity to chamomile, a commonly used infusion, resulting in allergic symptoms. Similarly, individuals with gastrointestinal sensitivities may find that even mild botanical infusions, such as peppermint, exacerbate symptoms like heartburn or reflux.
The importance of recognizing these individual sensitivities stems from the fact that pregnancy inherently alters the maternal immune system and gastrointestinal function, potentially making pregnant individuals more susceptible to adverse reactions. Prior exposure to a specific herb does not guarantee future tolerance during pregnancy. Furthermore, the concentration of bioactive compounds in herbal infusions can vary depending on factors such as plant species, growing conditions, and preparation methods. Therefore, even infusions generally deemed safe require careful monitoring for potential adverse effects. Some individuals may also be more sensitive to certain constituents in herbal preparations due to genetic factors affecting metabolism or detoxification processes.
In conclusion, individual sensitivities represent a crucial consideration when assessing the suitability of consuming herbal infusions during pregnancy. The potential for idiosyncratic reactions necessitates a cautious and individualized approach, prioritizing open communication with healthcare providers. By carefully considering personal medical history, monitoring for adverse effects, and selecting products from reputable sources, individuals can mitigate the risks associated with botanical infusion consumption during gestation. The challenge lies in the inherent variability among individuals and the lack of comprehensive research on the effects of specific herbs in diverse populations. Addressing this requires larger-scale studies that account for individual differences and provide more nuanced guidance.
3. Dosage considerations
Dosage constitutes a critical determinant in the safety profile of plant-based infusions consumed during gestation. While some infusions are generally deemed safe in limited quantities, exceeding recommended dosages can increase the risk of adverse effects on both the pregnant individual and the developing fetus. For instance, ginger infusions, often used to alleviate morning sickness, may lead to heartburn or gastric irritation when consumed in excessive amounts. Similarly, chamomile infusions, consumed for relaxation, can potentially exert sedative effects that may not be desirable during certain times of the day or in conjunction with other medications. Dosage therefore is central.
The significance of dosage considerations stems from the fact that the concentration of bioactive compounds in plant-based infusions can vary significantly depending on factors such as plant variety, growing conditions, and preparation methods. This variability underscores the importance of adhering to recommended serving sizes and avoiding concentrated extracts or preparations without professional guidance. Furthermore, the physiological changes associated with pregnancy, such as altered metabolism and increased renal clearance, can influence the way the body processes and eliminates these bioactive compounds. Real-life examples could entail specific plants considered abortifacient if ingested in high dosage. Careful consideration is therefore required when evaluating effects of herbal teas ok during pregnancy.
In summary, dosage is paramount in evaluating the safety of botanical infusions during gestation. While certain herbal teas may be considered generally safe in moderate amounts, exceeding recommended dosages can potentiate adverse effects. Challenges arise from variations in plant composition and individual sensitivities. By prioritizing adherence to dosage recommendations, consulting with healthcare providers, and exercising caution with concentrated preparations, individuals can mitigate risks and promote optimal outcomes. Future research should focus on establishing evidence-based dosage guidelines for specific herbal infusions during pregnancy, taking into account individual factors and potential interactions with medications.
4. Potential interactions
The potential for interactions between botanical infusions and concurrently administered pharmaceuticals or pre-existing medical conditions represents a significant consideration when evaluating the safety of herbal teas during pregnancy. These interactions can alter the efficacy of medications, exacerbate existing health issues, or introduce novel adverse effects, thereby compromising maternal and fetal well-being.
- Drug Metabolism Interference
Certain botanical compounds can inhibit or induce cytochrome P450 enzymes, which are crucial for drug metabolism. This interference can lead to either increased drug concentrations, potentially causing toxicity, or decreased drug concentrations, reducing therapeutic efficacy. For example, St. John’s Wort, though not typically recommended during pregnancy, is a known CYP3A4 inducer and could reduce the effectiveness of certain medications if co-administered. A similar interaction, though less well-documented, could hypothetically occur with other herbal teas. This alteration in drug metabolism has implications for any pregnant person taking medication.
- Additive or Synergistic Effects
Herbal teas can exert their own pharmacological effects, which may add to or synergize with those of pharmaceutical drugs, leading to unintended consequences. For example, if a pregnant person is taking an anticoagulant medication, the consumption of herbal teas containing coumarin-like compounds (such as chamomile in high doses) could increase the risk of bleeding. These additive or synergistic effects can amplify the impact of herbal teas. Even seemingly benign herbal teas ok during pregnancy can pose risks when combined with other medications.
- Impact on Physiological Parameters
Some botanical infusions can influence physiological parameters such as blood pressure, heart rate, or blood glucose levels. These effects may interact with existing medical conditions or medications used to manage those conditions. For example, pregnant individuals with gestational diabetes need to carefully manage their blood glucose. Herbal teas with potential hypoglycemic effects could interfere with diabetes management. Therefore, it’s imperative to consider that effects of herbal teas ok during pregnancy could influence pre-existing conditions.
- Alteration of Nutrient Absorption
Certain compounds present in herbal teas can interfere with the absorption of essential nutrients. Tannins, for instance, can bind to iron, reducing its bioavailability. This is particularly relevant during pregnancy when iron requirements are increased. If a pregnant individual consumes herbal teas rich in tannins concurrently with iron supplements, it could compromise iron absorption. Interactions in nutrient absorptions must be factored into the consideration of herbal teas ok during pregnancy.
These potential interactions underscore the importance of open communication with healthcare providers regarding all herbal tea consumption during pregnancy. A thorough evaluation of potential drug-herb interactions, as well as an assessment of pre-existing medical conditions, can help to minimize risks and ensure the safe and effective use of both pharmaceuticals and botanical infusions. This careful consideration of potential interactions is essential for safely choosing herbal teas during pregnancy.
5. Source reliability
The reliability of the source from which botanical infusions are obtained constitutes a critical factor in assessing their safety during gestation. Contamination, misidentification of plant species, and inconsistencies in product standardization can pose significant risks to both the pregnant individual and the developing fetus. The absence of rigorous quality control measures and transparent sourcing practices can compromise the integrity of the product, potentially leading to the presence of harmful substances, such as heavy metals, pesticides, or adulterants. For example, if a product labeled as chamomile is sourced from an unreliable vendor with lax quality control, it could inadvertently contain other plant species with known abortifacient properties, thereby posing a direct threat to the pregnancy. These examples highlight how source reliability effects safe effects of herbal teas ok during pregnancy.
The importance of source reliability stems from the fact that pregnant individuals are particularly vulnerable to the adverse effects of toxins and contaminants due to physiological changes that can alter absorption, distribution, metabolism, and excretion of various substances. Furthermore, the developing fetus is exquisitely sensitive to environmental exposures during critical periods of organogenesis and development. The consequences of consuming a contaminated or misidentified herbal infusion can range from mild gastrointestinal distress to more severe outcomes such as birth defects or miscarriage. A real-world example is the presence of pyrrolizidine alkaloids (PAs) in certain herbal products, which can cause liver damage and are particularly harmful during pregnancy. Reliable sourcing helps in ensuring safety profiles when considering effects of herbal teas ok during pregnancy.
In summary, source reliability is an indispensable aspect of ensuring the safety of herbal infusions consumed during pregnancy. Challenges arise from the complexity of the herbal supply chain, the lack of stringent regulatory oversight in certain regions, and the potential for economically motivated adulteration. By prioritizing products from reputable manufacturers with transparent sourcing practices, adhering to third-party certifications, and consulting with healthcare professionals, individuals can mitigate the risks associated with unreliable herbal sources. The selection of herbal teas ok during pregnancy needs reliable sources. Further research should focus on developing robust quality control standards and traceability systems for herbal products to safeguard the health and well-being of pregnant individuals and their offspring.
6. Specific herb effects
The specific pharmacological actions of individual herbs constitute a foundational element in determining the safety and suitability of herbal teas during gestation. Understanding the potential effects of each herb on maternal physiology and fetal development is paramount to making informed decisions regarding their consumption. Lack of precise knowledge can lead to unexpected and potentially harmful outcomes.
- Teratogenic Potential
Certain herbs possess teratogenic properties, meaning they can cause developmental abnormalities or birth defects. For example, pennyroyal contains pulegone, a compound known to induce uterine contractions and potentially cause miscarriage or birth defects. Therefore, herbal teas containing pennyroyal are contraindicated during pregnancy. Evaluating teratogenic potential is crucial when considering the effects of specific herbs, as even small amounts can pose a risk during critical stages of fetal development.
- Uterine Activity Modulation
Several herbs can affect uterine contractility, either stimulating or inhibiting uterine contractions. Herbs with stimulant properties, such as blue cohosh, can increase the risk of preterm labor or miscarriage. Conversely, other herbs may inhibit uterine contractions, potentially interfering with normal labor progression. Careful consideration of the effect on the uterus is vital. This modulation underscores the need for healthcare professional consultation when pregnant, as some have potential risks.
- Hormonal Influence
Certain herbs exert hormonal effects, either mimicking or interfering with endogenous hormone activity. For example, black cohosh, often used to alleviate menopausal symptoms, possesses estrogenic properties and may disrupt hormonal balance during pregnancy, potentially affecting fetal development. The evaluation is essential given the delicate hormonal interplay involved in maintaining pregnancy.
- Interaction with Maternal Physiology
Herbs can influence maternal physiological parameters, such as blood pressure, blood glucose levels, and blood coagulation. For instance, licorice root can elevate blood pressure due to its mineralocorticoid activity, posing a risk for pregnant individuals with hypertension. Similarly, herbs with anticoagulant properties can increase the risk of bleeding. Understanding potential interactions is critical for making informed choices, ensuring that maternal health is not compromised while considering any consumption of herbal teas.
The effects of specific herbs are a multifaceted consideration when evaluating the suitability of herbal teas during pregnancy. Factors such as teratogenic potential, influence on uterine activity, hormonal effects, and interactions with maternal physiology must be carefully assessed to minimize risks and promote favorable outcomes. Reliance on evidence-based information and consultation with healthcare professionals are indispensable for making informed decisions regarding herbal tea consumption during gestation.
Frequently Asked Questions
This section addresses common inquiries regarding the use of plant-based infusions during gestation. The information presented is intended to provide clarity and guidance; however, it should not replace consultation with a qualified healthcare professional.
Question 1: Is there a definitive list of herbal infusions considered universally safe throughout pregnancy?
No. The safety of an infusion depends on various factors, including the specific plant, its concentration, individual sensitivities, and the stage of gestation. While some plants are generally considered low-risk, no infusion is entirely without potential for adverse effects. Consultation with a healthcare provider is crucial.
Question 2: Are commercially available “pregnancy teas” inherently safe?
Not necessarily. The term “pregnancy tea” is not a regulated designation, and the composition of these products can vary widely. Scrutinize the ingredients list carefully and research each plant individually. Professional medical advice remains paramount.
Question 3: If an herbal infusion is labeled as “natural,” does that guarantee its safety during pregnancy?
No. The term “natural” does not equate to safety. Many plants contain potent bioactive compounds that can exert adverse effects, particularly during pregnancy. A thorough understanding of each plant’s properties is essential.
Question 4: Can herbal infusions interact with prescription medications during pregnancy?
Yes. Certain plants can interact with pharmaceutical drugs, altering their efficacy or increasing the risk of side effects. It is imperative to inform healthcare providers of all herbal infusions consumed to prevent potential adverse interactions.
Question 5: What is the significance of sourcing in relation to herbal infusion safety during pregnancy?
The source of the herbs is crucial. Products from reputable manufacturers with transparent sourcing practices are preferable. This minimizes the risk of contamination, misidentification of plant species, and inconsistencies in product standardization.
Question 6: If a healthcare provider is unfamiliar with herbal medicine, how can one obtain reliable information?
Seek consultation with a qualified herbalist or naturopathic physician with expertise in prenatal care. These professionals can provide individualized guidance based on a comprehensive assessment of individual needs and risk factors.
In summary, the use of herbal infusions during pregnancy requires a cautious and informed approach. Individual factors, plant properties, and sourcing practices all contribute to the overall safety profile.
The next section will explore specific plants frequently encountered in herbal infusions, categorizing them according to their generally recognized safety profiles during gestation.
Herbal Teas Ok During Pregnancy
This exploration has illuminated the complexities surrounding the consumption of herbal teas during gestation. The safety of such beverages is not a matter of blanket assurances, but rather a nuanced assessment contingent upon individual factors, specific herb properties, reliable sourcing, and potential interactions. Dosage considerations, individual sensitivities, and pre-existing medical conditions all contribute to the overall risk profile. The inherent variability in plant composition and the potential for contamination further necessitate cautious and informed decision-making. Ultimately, the absence of definitive proof of harm does not equate to guaranteed safety, underscoring the need for prudence.
Given the potential for both benefit and risk, a proactive and informed approach is essential. The judicious use of plant-based infusions during pregnancy demands open communication with healthcare providers, a commitment to evidence-based information, and a willingness to prioritize maternal and fetal well-being above unsubstantiated claims or anecdotal evidence. Future research should focus on elucidating the specific effects of individual herbs during pregnancy, establishing evidence-based dosage guidelines, and developing robust quality control standards for herbal products. Only through such rigorous investigation can the potential benefits of herbal teas be safely harnessed while minimizing risks to this vulnerable population.