Small intestinal bacterial overgrowth (SIBO) occurs when there is an excessive amount of bacteria in the small intestine. In cases where hydrogen-producing bacteria are prevalent, it is characterized as the hydrogen-dominant subtype. This specific manifestation of SIBO often presents with symptoms such as bloating, gas, and abdominal discomfort. Management strategies sometimes involve the use of natural remedies derived from plants to address the bacterial imbalance.
The appeal of employing botanical compounds in the management of this condition stems from their potential to offer antimicrobial effects while potentially minimizing the side effects associated with conventional antibiotic treatments. Historically, various cultures have utilized herbs for digestive ailments. The integration of these traditional approaches into modern practices reflects a growing interest in holistic and patient-centered care, aiming to improve gut health and alleviate associated symptoms.
Subsequent discussions will delve into the specific botanical agents that have shown promise in modulating the gut microbiome and reducing hydrogen production within the small intestine. It will also explore their mechanisms of action, dosage considerations, and potential synergistic effects when used in combination. Furthermore, the importance of dietary modifications and lifestyle adjustments alongside these interventions will be highlighted.
Guidance on Addressing Hydrogen-Dominant Small Intestinal Bacterial Overgrowth with Botanical Interventions
The following recommendations provide insights into the utilization of plant-derived substances for managing excessive hydrogen production in the small intestine due to bacterial overgrowth. These suggestions are intended to support informed decision-making in collaboration with a qualified healthcare provider.
Tip 1: Conduct Comprehensive Diagnostic Testing: Prior to initiating any intervention, confirm the presence of bacterial overgrowth and identify hydrogen dominance via breath testing. This diagnostic step is essential for tailoring treatment strategies.
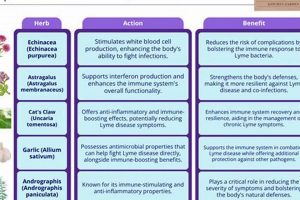
Tip 2: Select Targeted Antimicrobials: Investigate the application of botanical agents with demonstrated antimicrobial properties against common bacterial strains associated with SIBO. Examples include oregano oil, berberine, and allicin.
Tip 3: Implement a Low-FODMAP Diet: Minimize the consumption of fermentable carbohydrates (FODMAPs) to reduce the substrate available for bacterial fermentation and subsequent hydrogen production. Consult a registered dietitian for guidance.
Tip 4: Consider Prokinetic Agents: Evaluate the use of prokinetic herbs or medications to enhance gastrointestinal motility and prevent bacterial stasis in the small intestine. Ginger and Iberogast are potential options, but require medical evaluation.
Tip 5: Address Underlying Root Causes: Investigate and manage any underlying conditions contributing to the bacterial imbalance, such as low stomach acid, pancreatic enzyme insufficiency, or anatomical abnormalities.
Tip 6: Monitor for Die-Off Symptoms: Anticipate potential Herxheimer reactions (die-off symptoms) during the initial phase of antimicrobial treatment. These may include fatigue, headache, or flu-like symptoms. Support detoxification pathways with adequate hydration and liver-supportive herbs under professional guidance.
Tip 7: Implement Post-Treatment Support: Following antimicrobial therapy, focus on restoring gut health with probiotics and prebiotics to promote a balanced microbiome. This step is crucial for preventing recurrence.
Adherence to these recommendations, alongside professional medical guidance, can improve the chances of effectively managing the disorder and mitigating associated symptoms. It should be regarded as a component of a comprehensive, tailored therapeutic approach.
The concluding sections will further elaborate on the long-term strategies to maintain gut health and prevent future occurrences of the aforementioned imbalance.
1. Antimicrobial properties
The core strategy in addressing hydrogen-dominant small intestinal bacterial overgrowth involves reducing the excessive bacterial population within the small intestine. Plant-derived compounds exhibiting antimicrobial properties serve as a primary therapeutic modality in this approach. These substances target and inhibit the growth of bacteria responsible for excessive hydrogen production, thereby alleviating associated symptoms such as bloating, gas, and abdominal discomfort. For example, berberine, found in plants like goldenseal and barberry, demonstrates broad-spectrum antibacterial activity, disrupting bacterial cell walls and inhibiting metabolic processes. Similarly, allicin, derived from garlic, exhibits potent antibacterial effects through inhibiting enzymes essential for bacterial survival. The selection of specific herbal antimicrobials is contingent upon the specific bacterial species implicated in the overgrowth, typically determined through breath testing or stool analysis.
The efficacy of antimicrobial agents in managing the condition is contingent upon several factors, including dosage, duration of treatment, and the specific formulation of the herbal extract. Overuse or inappropriate use can lead to bacterial resistance and dysbiosis, underscoring the importance of employing these substances under the guidance of a qualified healthcare practitioner. Furthermore, combining antimicrobial herbs with other therapeutic interventions, such as dietary modifications (e.g., a low-FODMAP diet) and prokinetic agents, can enhance treatment outcomes. Clinical studies have shown that herbal antimicrobial protocols can effectively reduce hydrogen levels in breath tests and improve symptom scores in individuals with the condition.
In summary, the application of herbal agents with antimicrobial properties is a critical component in the management of hydrogen-dominant small intestinal bacterial overgrowth. These substances target and inhibit the growth of bacteria responsible for excessive hydrogen production. While efficacious, their use necessitates careful consideration of dosage, duration, and potential side effects, emphasizing the importance of professional medical guidance. The integration of antimicrobial herbs within a comprehensive treatment plan, including dietary modifications and prokinetic agents, maximizes the likelihood of successful outcomes and sustained symptom relief. Challenges include potential bacterial resistance and the need for accurate diagnostic testing to identify the specific bacterial species involved, highlighting the need for ongoing research in this area.
2. Gut Motility
Gut motility, referring to the coordinated contractions of the gastrointestinal tract that propel its contents, plays a crucial role in the context of hydrogen-dominant small intestinal bacterial overgrowth and its botanical management. Impaired motility can contribute to bacterial stasis in the small intestine, fostering an environment conducive to bacterial overgrowth and subsequent hydrogen production.
- Mechanism of Bacterial Stasis
Reduced gut motility creates an environment where bacteria can accumulate in the small intestine. This stasis provides a longer residence time for bacteria to ferment undigested carbohydrates, leading to increased hydrogen production. For example, conditions like gastroparesis or chronic constipation can significantly impair gut motility, increasing the risk of SIBO development.
- Impact on Herbal Treatment Efficacy
Herbal treatments aimed at reducing bacterial overgrowth may be less effective if gut motility is compromised. The slowed transit time allows bacteria to repopulate more rapidly after antimicrobial treatment. Some herbal remedies, such as prokinetic agents like ginger, can simultaneously address both the bacterial overgrowth and the underlying motility issues.
- Role of Prokinetic Herbs
Prokinetic herbs stimulate gastrointestinal motility, helping to clear bacteria from the small intestine and prevent stasis. Ginger, Iberogast, and artichoke extract are examples of herbal agents with prokinetic properties. These substances act on various receptors and pathways in the gut to enhance peristalsis, promoting the forward movement of intestinal contents.
- Importance of Integrated Management
Addressing impaired gut motility is integral to the successful management of hydrogen-dominant SIBO. A comprehensive approach incorporates both antimicrobial agents to reduce the bacterial load and prokinetic agents to improve gut transit time. Ignoring motility issues can lead to recurrent SIBO and persistent symptoms, even with effective antimicrobial therapy.
The connection between gut motility and hydrogen-dominant SIBO underscores the necessity of a holistic treatment strategy. Addressing motility deficits alongside targeted antimicrobial interventions is paramount to achieving sustained relief from SIBO and preventing its recurrence. The synergistic application of herbal remedies targeting both bacterial overgrowth and gut motility represents a promising avenue for managing this condition.
3. Hydrogen reduction
In hydrogen-dominant small intestinal bacterial overgrowth, an excess of bacteria in the small intestine leads to increased fermentation of undigested carbohydrates, resulting in elevated hydrogen production. This excess hydrogen contributes to the characteristic symptoms of SIBO, such as bloating, gas, and abdominal discomfort. Consequently, the effective management of hydrogen-dominant SIBO necessitates strategies focused on curtailing hydrogen production within the gut. These strategies may involve botanical interventions that target the underlying bacterial overgrowth or directly inhibit the enzymatic processes responsible for hydrogen generation. For example, specific herbs may exert antimicrobial effects on hydrogen-producing bacteria, reducing their overall population and, thereby, hydrogen output.
Certain plant-derived compounds can influence the metabolic pathways within the gut microbiome, diminishing hydrogen production. Some herbs might compete with bacteria for available substrates or alter the gut environment to disfavor hydrogen-producing species. Furthermore, reducing dietary intake of fermentable carbohydrates (FODMAPs) is a dietary modification that complements these herbal interventions. By limiting the available substrate for bacterial fermentation, dietary changes directly reduce the potential for hydrogen production, augmenting the effect of botanical treatments aimed at modulating the bacterial population. The practical significance lies in the potential for a synergistic effect: herbal interventions targeting the source of hydrogen production combined with dietary restrictions on substrate availability.
Therefore, the successful management of hydrogen-dominant small intestinal bacterial overgrowth involves a comprehensive approach that considers both the bacterial overgrowth and the subsequent hydrogen production. Herbal interventions, when thoughtfully integrated with dietary modifications, offer a means to achieve significant hydrogen reduction. Challenges remain in identifying the most effective botanical agents and tailoring treatment plans to individual patients based on their unique microbiome composition and dietary sensitivities. Ongoing research aims to refine these therapeutic strategies, further optimizing the use of herbal treatments for hydrogen reduction in individuals with hydrogen-dominant SIBO.
4. Inflammation control
Control of inflammation is a critical aspect of managing hydrogen-dominant small intestinal bacterial overgrowth. The excessive bacterial fermentation characteristic of this condition often triggers inflammatory responses within the gut, exacerbating symptoms and potentially contributing to long-term complications. Therefore, therapeutic strategies targeting inflammation are integral to a comprehensive treatment approach alongside efforts to reduce bacterial overgrowth.
- Intestinal Permeability
The chronic inflammation associated with SIBO can compromise the integrity of the intestinal lining, leading to increased permeability, often referred to as “leaky gut.” This allows bacterial products and other inflammatory substances to enter the bloodstream, triggering systemic inflammation. Herbal interventions that promote gut barrier function, such as those containing glutamine or zinc carnosine, can help mitigate this effect.
- Immune System Modulation
The inflammatory response in SIBO is mediated by the immune system. Certain botanical agents possess immunomodulatory properties, helping to balance the immune response and reduce excessive inflammation. For example, curcumin, derived from turmeric, has demonstrated anti-inflammatory effects by inhibiting key inflammatory pathways. Similarly, chamomile can soothe the intestinal lining and reduce inflammation through its antioxidant and anti-inflammatory compounds.
- Reduction of Pro-inflammatory Cytokines
The inflammatory process in SIBO involves the release of pro-inflammatory cytokines, such as TNF-alpha and IL-6. Herbal interventions can help suppress the production and activity of these cytokines. For instance, Boswellia serrata, also known as frankincense, contains compounds that inhibit the production of leukotrienes, inflammatory mediators that contribute to gut inflammation.
- Antioxidant Support
Chronic inflammation generates oxidative stress, which can further damage the intestinal lining and exacerbate inflammation. Antioxidant-rich herbs can help neutralize free radicals and reduce oxidative damage. Examples include green tea extract, which contains polyphenols with potent antioxidant properties, and ginger, which contains compounds that combat oxidative stress and inflammation.
The multifaceted benefits of inflammation control within the context of hydrogen-dominant SIBO underscore the importance of incorporating targeted herbal strategies into comprehensive treatment plans. By addressing inflammation, these interventions aim to alleviate symptoms, improve gut barrier function, modulate the immune system, and protect against oxidative damage. This holistic approach enhances the overall efficacy of SIBO management and promotes long-term gut health.
5. Microbiome balance
Achieving and maintaining microbiome balance is a central objective in the context of hydrogen-dominant small intestinal bacterial overgrowth and its herbal management. Eradicating bacterial overgrowth without fostering a balanced microbial ecosystem within the gut can lead to recurrence and other digestive disturbances. Herbal treatments, therefore, should not only target the reduction of excessive hydrogen-producing bacteria but also support the restoration of a healthy and diverse gut microbiome.
- Selective Antimicrobial Action
Ideal herbal antimicrobials exhibit selective action, targeting pathogenic bacteria while preserving beneficial species. Broad-spectrum antibiotics can disrupt the entire gut microbiome, potentially leading to fungal overgrowth or colonization by opportunistic pathogens. Berberine, for example, has demonstrated antimicrobial activity against various bacteria, but its effect on beneficial species requires careful consideration. The goal is to reduce the population of hydrogen producers without significantly harming the overall microbial diversity.
- Probiotic Support Post-Treatment
Following antimicrobial herbal treatment, probiotic supplementation can aid in repopulating the gut with beneficial bacteria. Probiotics containing strains such as Lactobacillus and Bifidobacterium can improve gut barrier function, reduce inflammation, and compete with remaining pathogenic bacteria. The selection of specific probiotic strains should be guided by the individual’s microbiome profile and symptom presentation.
- Prebiotic Integration
Prebiotics, non-digestible fibers that promote the growth of beneficial bacteria, also play a role in microbiome balance. Incorporating prebiotic-rich foods or supplements can nourish beneficial bacterial populations, encouraging their proliferation and contributing to a more diverse and resilient gut ecosystem. Examples include inulin, fructooligosaccharides (FOS), and galactooligosaccharides (GOS).
- Modulation of Gut Environment
Certain herbs can indirectly support microbiome balance by modulating the gut environment. For example, herbs that reduce inflammation, such as chamomile or ginger, can create a more hospitable environment for beneficial bacteria to thrive. Similarly, herbs that improve gut motility can prevent bacterial stasis, reducing the risk of overgrowth and promoting a more balanced microbial distribution throughout the digestive tract.
The emphasis on microbiome balance in the herbal management of hydrogen-dominant small intestinal bacterial overgrowth reflects a broader understanding of gut health and its impact on overall well-being. A holistic approach that addresses both the reduction of overgrowth and the restoration of a healthy microbial ecosystem offers the best chance for long-term symptom relief and improved digestive function.
6. Dietary Synergy
The efficacy of herbal interventions for hydrogen-dominant small intestinal bacterial overgrowth is significantly influenced by concurrent dietary strategies. Dietary synergy, in this context, refers to the amplified therapeutic benefit achieved when specific dietary modifications are combined with herbal treatments. Certain dietary approaches, particularly those that limit fermentable carbohydrates, reduce the substrate available for bacterial fermentation, thereby decreasing hydrogen production. This effect complements the antimicrobial actions of herbal agents, which aim to reduce the bacterial population itself. For instance, a low-FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) diet restricts the intake of carbohydrates that are readily fermented by bacteria in the small intestine. When implemented alongside herbal antimicrobials such as berberine or oregano oil, this dietary approach can lead to a more pronounced reduction in hydrogen levels and associated symptoms than either intervention alone.
Practical application of dietary synergy requires a tailored approach, considering individual tolerance levels and dietary preferences. While a low-FODMAP diet is commonly recommended, some individuals may benefit from additional restrictions, such as limiting specific sugars or starches. Working with a registered dietitian or nutritionist is crucial to develop a personalized dietary plan that aligns with the herbal treatment regimen. Furthermore, dietary strategies can also support gut healing and reduce inflammation, further enhancing the benefits of herbal interventions. For example, incorporating anti-inflammatory foods like ginger and turmeric, or consuming L-glutamine to support intestinal barrier function, can augment the therapeutic effects of herbal antimicrobials. Real-world applications involve patients who experience persistent symptoms despite herbal treatment alone finding significant relief when adhering to a well-structured, personalized low-FODMAP diet.
In summary, dietary synergy represents a critical component of hydrogen-dominant small intestinal bacterial overgrowth management. Combining specific dietary modifications with herbal treatments leverages their complementary mechanisms of action, resulting in improved symptom control and enhanced treatment outcomes. While challenges exist in tailoring dietary plans to individual needs and tolerances, the potential benefits of dietary synergy underscore its importance in a comprehensive therapeutic approach. Ongoing research continues to explore the optimal dietary strategies to maximize the effectiveness of herbal interventions for this condition.
7. Long-term maintenance
Long-term maintenance is a critical, often overlooked, component of successful management of hydrogen-dominant small intestinal bacterial overgrowth. While herbal treatments can effectively reduce bacterial overgrowth and alleviate acute symptoms, these interventions do not address the underlying causes that predispose individuals to the condition. Consequently, without a structured maintenance plan, recurrence is highly probable. The effectiveness of herbal treatments is contingent upon a concurrent strategy to prevent bacterial resurgence.
Maintenance protocols typically involve several key elements: dietary modifications, prokinetic agents, and intermittent use of antimicrobial herbs. Dietary adjustments, such as a modified low-FODMAP diet or specific carbohydrate restrictions, limit the availability of substrates for bacterial fermentation, reducing hydrogen production. Prokinetic agents, whether pharmaceutical or herbal (e.g., ginger), promote gut motility, preventing bacterial stasis in the small intestine. Intermittent use of antimicrobial herbs, at lower doses than those used during initial treatment, helps to suppress bacterial growth and maintain a balanced gut microbiome. For example, an individual who successfully eradicated SIBO with berberine may take a maintenance dose of berberine for one week each month to prevent recurrence. Lifestyle factors, such as stress management and adequate sleep, also play a significant role in supporting long-term gut health.
The ultimate goal of long-term maintenance is to address the root causes that contributed to the initial bacterial overgrowth. This may involve identifying and managing underlying conditions such as hypochlorhydria, pancreatic enzyme insufficiency, or structural abnormalities in the small intestine. Without addressing these factors, even the most diligent maintenance plan may prove insufficient. Therefore, long-term maintenance represents an individualized, proactive approach to sustaining gut health and preventing SIBO recurrence, requiring ongoing collaboration between the patient and healthcare provider. Adherence to a tailored plan will allow for the full potential of herbal treatment of SIBO to be realized.
Frequently Asked Questions
The following questions address common concerns and misconceptions surrounding the management of hydrogen-dominant small intestinal bacterial overgrowth (SIBO) with herbal therapies. The information presented is intended for educational purposes and should not substitute professional medical advice.
Question 1: Are herbal treatments a proven cure for hydrogen-dominant SIBO?
Herbal treatments can effectively reduce bacterial overgrowth and alleviate symptoms in many individuals with hydrogen-dominant SIBO. However, the term “cure” requires careful consideration. While herbal therapies can induce remission, they do not always address the underlying causes of SIBO, which can lead to recurrence. A comprehensive approach that addresses both the overgrowth and its root causes is essential.
Question 2: What are the most effective herbal antimicrobials for hydrogen-dominant SIBO?
Several herbal antimicrobials have demonstrated efficacy against bacteria commonly associated with hydrogen-dominant SIBO. These include berberine (found in plants like goldenseal and barberry), allicin (derived from garlic), oregano oil, and neem. The choice of specific herbs depends on individual factors, such as symptom presentation, gut microbiome composition, and potential drug interactions.
Question 3: Are herbal treatments safe for everyone with hydrogen-dominant SIBO?
Herbal treatments are generally considered safe when used appropriately and under the guidance of a qualified healthcare practitioner. However, some individuals may experience side effects, such as digestive upset or allergic reactions. Certain herbs may also interact with prescription medications. Pregnant or breastfeeding women should exercise caution and seek professional medical advice before using herbal therapies.
Question 4: How long does it take to see results with herbal treatment for hydrogen-dominant SIBO?
The time required to see results varies depending on the severity of the SIBO, the specific herbal protocol used, and individual factors. Some individuals may experience symptom improvement within a few weeks, while others may require several months of treatment. Consistent adherence to the treatment plan, including dietary modifications and lifestyle adjustments, is crucial for optimal outcomes.
Question 5: Can dietary modifications alone resolve hydrogen-dominant SIBO?
Dietary modifications, such as a low-FODMAP diet, can effectively manage symptoms and reduce hydrogen production in many individuals with hydrogen-dominant SIBO. However, dietary changes alone may not completely eradicate the bacterial overgrowth. A combination of dietary modifications and herbal antimicrobials often yields the best results.
Question 6: What is the role of prokinetic agents in the herbal treatment of hydrogen-dominant SIBO?
Prokinetic agents, which promote gut motility, play a crucial role in preventing bacterial stasis and recurrence of SIBO. Herbal prokinetics, such as ginger and Iberogast, can enhance the efficacy of antimicrobial treatments by facilitating the clearance of bacteria from the small intestine.
The successful management of this condition with herbal approaches often requires a comprehensive and individualized strategy. Consulting with a healthcare professional experienced in SIBO is essential for developing a safe and effective treatment plan.
The subsequent sections will explore specific considerations for individualized herbal protocols and potential challenges encountered during treatment.
Conclusion
The exploration of `hydrogen dominant sibo herbal treatment` reveals a complex landscape requiring careful consideration. Botanical interventions offer a potential avenue for managing the bacterial overgrowth and associated symptoms. However, success hinges on accurate diagnosis, targeted antimicrobial selection, attention to gut motility, and dietary synergy. Furthermore, long-term maintenance strategies are paramount to preventing recurrence.
The information underscores the need for a holistic approach to `hydrogen dominant sibo herbal treatment`. Individuals considering this path must engage with qualified healthcare practitioners to develop personalized plans. Further research is essential to refine treatment protocols and validate the long-term efficacy of herbal therapies in this challenging condition.