The integration of botanical remedies to combat fungal infections represents a long-standing practice across various cultures. This approach employs plant-derived compounds, often in the form of extracts, tinctures, or topical applications, to inhibit fungal growth or alleviate associated symptoms. For instance, tea tree oil, derived from the Australian Melaleuca alternifolia tree, is frequently utilized for its documented antifungal properties in treating conditions such as athlete’s foot.
The significance of employing plant-based interventions for fungal ailments lies in the potential for accessible and affordable care, particularly in regions where conventional pharmaceuticals are scarce or prohibitively expensive. Historically, many traditional medicinal systems have relied on readily available plant resources to manage a range of health conditions, including those caused by fungal pathogens. The advantages can extend to a lower risk of side effects compared to some synthetic drugs, although rigorous scientific evaluation remains essential.
The following discussion will delve into specific botanical agents that have demonstrated potential in addressing fungal infections, examining their mechanisms of action, current research findings, and the overall role of complementary therapies in the management of these prevalent health concerns. Subsequent sections will also address safety considerations and the importance of consulting with qualified healthcare professionals before initiating any self-treatment regimen.
Guidance on Botanical Approaches to Fungal Management
The subsequent recommendations provide information regarding the integration of botanical remedies for fungal infections. It is imperative to understand that these suggestions are for informational purposes only and do not constitute medical advice. Consultation with a qualified healthcare professional is essential before initiating any new treatment protocol.
Tip 1: Identify the Specific Fungal Infection. Accurate identification of the fungal pathogen is crucial. Different fungal species respond differently to various botanical agents. Laboratory testing may be necessary to determine the precise cause of the infection.
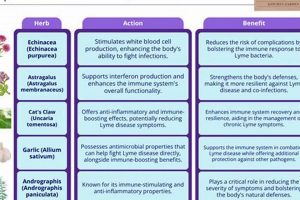
Tip 2: Select Appropriate Botanical Agents. Research the documented antifungal properties of various herbs. Examples include tea tree oil ( Melaleuca alternifolia), garlic ( Allium sativum), and oregano oil ( Origanum vulgare). Ensure the chosen herb has demonstrated efficacy against the identified fungal species.
Tip 3: Ensure Proper Preparation and Dosage. Adhere strictly to recommended dosages and preparation methods. Plant extracts and essential oils vary in concentration; therefore, follow established guidelines to minimize the risk of adverse reactions or ineffectiveness.
Tip 4: Implement Consistent Application or Ingestion. Regular and consistent application or ingestion is paramount for achieving therapeutic benefits. Fungal infections often require sustained treatment periods for complete eradication. Missed applications or inconsistent dosages can impede progress.
Tip 5: Monitor for Allergic Reactions or Adverse Effects. Closely monitor for any signs of allergic reactions or adverse effects. Discontinue use immediately if irritation, rash, or other unfavorable symptoms develop. Some individuals may exhibit sensitivity to certain botanical compounds.
Tip 6: Practice Proper Hygiene. Maintain rigorous hygiene practices to prevent the spread or recurrence of fungal infections. This includes regular washing with soap and water, keeping affected areas dry, and avoiding sharing personal items.
Tip 7: Consider Combining Botanical Remedies with Conventional Treatments. In certain cases, a combined approach involving both botanical and conventional antifungal medications may be beneficial. However, this should only be undertaken under the guidance of a healthcare professional to avoid potential drug interactions.
The judicious use of botanical resources can potentially offer a valuable adjunct in the management of fungal ailments. However, safety, efficacy, and appropriate application remain paramount considerations. The presented guidance underscores the significance of responsible and informed decision-making in incorporating plant-based approaches into a comprehensive healthcare strategy.
The following section will explore the integration of botanical approaches within a holistic framework of health management and preventative care.
1. Identification.
The successful application of botanical remedies for fungal infections hinges critically on accurate identification of the causative fungal species. Different fungi exhibit varying sensitivities to different herbal constituents; therefore, broad-spectrum, uninformed applications are unlikely to yield optimal results and may promote resistance. Precise identification enables a targeted approach, ensuring the selected herbal treatment possesses specific antifungal activity against the identified pathogen. For example, Candida albicans, a common cause of yeast infections, may respond favorably to caprylic acid found in coconut oil, while Trichophyton rubrum, frequently associated with athlete’s foot, may be more susceptible to tea tree oil.
Failure to accurately identify the responsible fungal species can lead to ineffective treatment, prolonged infection duration, and potential complications. Consider a scenario where a patient self-treats a nail infection with an herbal remedy intended for athlete’s foot; if the nail infection is caused by a different fungal species, the chosen herbal application will likely prove futile, allowing the infection to progress and potentially requiring more aggressive intervention later. Similarly, misidentification can mask underlying conditions that predispose an individual to fungal infections, hindering efforts to address root causes and prevent recurrence.
In summary, precise identification stands as a cornerstone of effective herbal treatment for fungal infections. It guides the selection of appropriate herbal agents, maximizes treatment efficacy, prevents prolonged infections, and minimizes the risk of complications. The practical significance of this understanding underscores the necessity for professional diagnostic testing to inform targeted herbal treatment strategies, particularly in cases of persistent or severe fungal infections.
2. Herb Selection
The selection of appropriate herbs constitutes a crucial determinant of success in addressing fungal infections using botanical remedies. Effective treatment necessitates identifying herbs possessing demonstrated antifungal activity against the specific fungal pathogen identified through diagnostic testing. For instance, the use of tea tree oil, known for its antifungal properties, may prove beneficial for treating athlete’s foot caused by Trichophyton species, while its efficacy against systemic fungal infections would be limited. The causal link between herb selection and treatment outcome underscores the importance of informed decision-making in this process. The absence of targeted antifungal activity renders the treatment ineffective, potentially exacerbating the infection or leading to the development of resistance.
The importance of herb selection extends beyond mere antifungal properties to encompass considerations of bioavailability, safety, and potential interactions with other medications. Some herbal constituents may exhibit potent antifungal activity in vitro but demonstrate poor absorption or rapid metabolism in vivo, limiting their therapeutic potential. Furthermore, certain herbs may pose risks of adverse effects or interact negatively with conventional antifungal drugs, necessitating careful evaluation and professional guidance. As an example, grapefruit juice, while not an antifungal herb itself, is known to interact with several antifungal medications, altering their serum concentrations and potentially leading to toxicity or treatment failure. Careful selection and use are a must and crucial to patient saftey.
In summary, herb selection represents an indispensable component of effective fungus herbal treatment. The practical significance of this understanding lies in the ability to tailor treatment strategies based on scientific evidence and individual patient needs, maximizing the likelihood of positive outcomes while minimizing potential risks. The presented analysis emphasizes the importance of professional consultation and evidence-based decision-making in harnessing the therapeutic potential of botanical remedies for fungal infections. Herb selection is therefore a fundamental and crucial step in a fungus herbal treatment.
3. Preparation Method
The preparation method employed significantly influences the efficacy of a fungus herbal treatment. The method determines the extraction and preservation of bioactive compounds within the herb, directly impacting its antifungal potency. Improper preparation may render the herb ineffective, even if it possesses inherent antifungal properties. For example, preparing a weak tea from a herb requiring decoction will fail to extract sufficient active constituents to combat a fungal infection. Similarly, improper drying or storage can degrade the active compounds, diminishing the herb’s therapeutic value. Therefore, selecting and executing the correct preparation method is not merely procedural but functionally crucial to the success of a fungus herbal treatment.
Specific preparation techniques, such as tincturing, poultice application, or steam inhalation, cater to different herb properties and routes of administration. Tincturing, involving extraction with alcohol, effectively concentrates non-polar antifungal compounds. A poultice allows direct application of fresh or dried herbs to localized fungal infections on the skin. Steam inhalation facilitates the delivery of volatile antifungal compounds to the respiratory tract. The failure to choose a suitable method reduces the bioavailability of the active compounds, thereby hindering their ability to interact with the fungal pathogen. The selection must be grounded in the chemical properties of the desired antifungal constituents and the nature of the fungal infection. Consider a topical application to the skin: the type of carrier oil used, as well as any added compounds to promote absorption, is essential for the herbal agents to reach the fungal colonies. For ingestion, the process must not only extract the compound, but also ensure it is bioavailable enough to be digested and still reach the infection sites.
In summary, the preparation method constitutes a critical, non-negotiable component of effective fungus herbal treatment. Inappropriate or inadequate preparation undermines the therapeutic potential of even the most potent antifungal herbs. The presented analysis emphasizes the essential role of informed and precise preparation in achieving favorable outcomes, underscoring the need for adherence to established protocols and, when necessary, consultation with experienced herbalists or healthcare practitioners. Proper preparation is not an optional adjunct but an indispensable step in realizing the benefits of herbal approaches to managing fungal infections and requires a careful process.
4. Dosage Accuracy
The administration of herbal remedies for fungal infections necessitates precise adherence to established dosage guidelines. Dosage accuracy forms a critical pillar of effective and safe fungus herbal treatment. Insufficient dosages may fail to inhibit fungal growth or alleviate symptoms, rendering the treatment ineffective and potentially fostering fungal resistance. Conversely, excessive dosages can lead to adverse effects, ranging from mild gastrointestinal distress to more severe systemic reactions. The inherent variability in the concentration of active compounds within herbal products further underscores the importance of meticulous attention to dosage, as even seemingly identical preparations may exhibit differing potencies. Dosage therefore is the fine balance in treating a fungal infection.
Real-world examples underscore the impact of dosage accuracy on treatment outcomes. For instance, garlic, often employed for its antifungal properties, requires careful dosing. While small amounts of garlic may offer some benefit, higher doses can cause digestive upset or even interfere with certain medications. Similarly, tea tree oil, commonly used topically, must be diluted appropriately to avoid skin irritation or allergic reactions. A failure to accurately measure or dilute these herbal remedies can negate their therapeutic potential or even cause harm. This principle extends to internal herbal medications as well: an inaccurate prescription, or even one not accurately measured by the patient, may lead to the treatment being less effective.
In summary, dosage accuracy constitutes a non-negotiable aspect of responsible and effective fungus herbal treatment. Maintaining an appropriate and carefully measured dose is of the utmost importance. Its influence permeates every stage of the treatment process, from initial symptom relief to sustained fungal eradication. By recognizing and prioritizing the significance of dosage accuracy, practitioners and patients alike can optimize the therapeutic potential of herbal remedies while minimizing the risk of adverse outcomes. A fungus herbal treatment requires a delicate balance of herbal selection and precise dosing for the best outcome, and this should be carefully considered.
5. Application Consistency.
The sustained effectiveness of fungus herbal treatment relies heavily on consistent application of the selected remedy. Eradicating fungal infections typically demands prolonged exposure to antifungal agents, whether derived from botanical or pharmaceutical sources. Inconsistent application provides fungal organisms with periods of reprieve, allowing for continued growth, adaptation, and potential development of resistance. Therefore, lapses in the prescribed application schedule directly compromise the treatment’s ability to achieve its intended outcome, underscoring application consistency as a foundational element of success.
Consider the treatment of onychomycosis (nail fungus) with topical herbal solutions. Effective management necessitates meticulous daily application of the chosen remedy, ensuring that the antifungal compounds penetrate the nail bed and reach the underlying fungal colonies. Intermittent application allows the surviving fungal organisms to re-establish themselves, effectively nullifying the progress made during periods of consistent treatment. A similar principle applies to the use of herbal washes or creams for cutaneous fungal infections. Irregular use reduces the duration of exposure to the antifungal agents, diminishing their capacity to eradicate the infection completely. The real-world consequences of inconsistent application translate to prolonged infection duration, increased risk of recurrence, and potential escalation to more aggressive treatment strategies.
In summary, application consistency serves as a critical determinant of success in fungus herbal treatment. The sustained suppression of fungal growth necessitates adherence to the prescribed application schedule, minimizing opportunities for fungal adaptation and proliferation. Recognizing the pivotal role of application consistency, both patients and healthcare providers can work collaboratively to establish realistic treatment regimens, reinforce adherence, and optimize the likelihood of achieving complete and lasting resolution of fungal infections. A consistent fungus herbal treatment ensures a better chance of success.
6. Hygiene Practices.
Hygiene practices exert a profound influence on the effectiveness of fungus herbal treatment, serving as both a preventative measure and a supportive component of the therapeutic regimen. Fungal infections often thrive in environments characterized by warmth, moisture, and compromised skin integrity. Consequently, meticulous hygiene practices minimize these conducive conditions, reducing the risk of initial infection and preventing the recurrence or spread of existing infections during treatment. The absence of appropriate hygiene can directly counteract the benefits of even the most potent herbal remedies.
The specific hygiene practices relevant to fungus herbal treatment vary depending on the type and location of the fungal infection. For cutaneous infections, regular washing with soap and water, thorough drying of the affected area, and avoidance of occlusive clothing are essential. In cases of athlete’s foot, wearing breathable footwear, changing socks frequently, and using antifungal powders contribute significantly to both treatment and prevention. Maintaining clean and dry conditions within shoes, for example, limits the fungal growth environment, thereby enhancing the efficacy of topical herbal applications. For vaginal yeast infections, avoiding douching and wearing breathable cotton underwear promotes a healthy vaginal flora and reduces the likelihood of recurrence. Furthermore, proper handwashing techniques are crucial in preventing the spread of fungal infections from one body part to another or to other individuals. Shared towels, socks, or other personal items can act as reservoirs for fungal spores, necessitating diligent hygiene to break the chain of transmission. The failure to adhere to these practices can impede the progress of herbal treatment and perpetuate the infection cycle. A comprehensive approach integrates herbal remedies with hygiene for optimal outcomes.
In summary, hygiene practices represent an indispensable element of comprehensive fungus herbal treatment. Their role extends beyond mere prevention, actively supporting the therapeutic action of herbal remedies by addressing the underlying environmental factors that contribute to fungal growth. Emphasizing and implementing appropriate hygiene measures significantly enhances the likelihood of successful treatment outcomes, reduces the risk of recurrence, and promotes overall well-being. Therefore, hygiene practices are vital to the efficacy of fungus herbal treatment.
7. Professional Guidance.
The integration of professional guidance constitutes a critical determinant in the safe and effective application of fungus herbal treatment. The inherent complexities associated with fungal infections, compounded by the nuanced knowledge required to select, prepare, and administer herbal remedies, necessitate expert oversight. Self-diagnosis and self-treatment, without the benefit of professional assessment, can lead to misidentification of the causative fungal species, inappropriate herb selection, improper dosage, and potential adverse interactions with existing medical conditions or medications. The causal relationship between informed professional guidance and successful treatment outcomes underscores its indispensability.
The importance of professional guidance extends beyond accurate diagnosis and treatment selection to encompass the monitoring of treatment progress and the management of potential complications. A qualified healthcare practitioner can assess the efficacy of the chosen herbal remedy, identify any adverse reactions, and adjust the treatment plan as needed. For example, if a patient experiences skin irritation or allergic reaction from a topical herbal application, a professional can advise on alternative remedies or strategies to mitigate the adverse effects. Furthermore, professional guidance is essential for patients with underlying health conditions or those taking other medications, as certain herbal remedies may interact negatively with conventional treatments. Professional guidance can also include the use of laboratory tests to verify diagnosis, select targeted therapies, and monitor progress in healing.
In summary, professional guidance represents a cornerstone of responsible and effective fungus herbal treatment. Its integration into the treatment process minimizes the risks associated with self-treatment, optimizes the selection and application of herbal remedies, and facilitates the monitoring of treatment progress and the management of potential complications. Prioritizing professional guidance enhances the safety and efficacy of fungus herbal treatment, promoting positive outcomes and minimizing the likelihood of adverse events. Therefore, seeking counsel from qualified healthcare professionals ensures that fungus herbal treatment is pursued safely and effectively.
Frequently Asked Questions About Fungus Herbal Treatment
The following addresses common inquiries regarding the use of botanical remedies for fungal infections, emphasizing the importance of informed decision-making and professional guidance.
Question 1: What constitutes “fungus herbal treatment”?
Fungus herbal treatment refers to the utilization of plant-derived substances, such as extracts, tinctures, or essential oils, to inhibit the growth of fungal pathogens or alleviate symptoms associated with fungal infections. This approach often draws upon traditional medicinal practices and contemporary scientific research to identify and apply botanicals with documented antifungal properties.
Question 2: Is fungus herbal treatment a suitable alternative to conventional antifungal medications?
Fungus herbal treatment may offer a complementary or adjunctive approach to conventional antifungal medications. However, it is generally not recommended as a sole alternative, particularly in cases of severe or systemic fungal infections. The efficacy of herbal remedies can vary depending on the fungal species, the severity of the infection, and individual patient factors. Consultation with a healthcare professional is crucial to determine the most appropriate treatment strategy.
Question 3: What are the potential risks associated with fungus herbal treatment?
Potential risks associated with fungus herbal treatment include allergic reactions, skin irritation, interactions with other medications, and the possibility of treatment failure if the chosen herbal remedy is ineffective against the specific fungal pathogen. Some herbal products may also contain contaminants or adulterants that can pose health risks. It is essential to source herbal remedies from reputable suppliers and to consult with a qualified healthcare practitioner before initiating treatment.
Question 4: How can one determine the appropriate dosage of herbal remedies for fungal infections?
Determining the appropriate dosage of herbal remedies requires careful consideration of several factors, including the specific herb, the form of the preparation (e.g., extract, tincture, essential oil), the severity of the infection, and individual patient characteristics. It is generally advisable to start with a low dose and gradually increase it as tolerated, while closely monitoring for any adverse effects. Consulting with a qualified herbalist or healthcare practitioner is highly recommended to ensure accurate dosing and to minimize the risk of side effects.
Question 5: How long does it typically take to see results from fungus herbal treatment?
The timeframe for observing results from fungus herbal treatment can vary significantly depending on the type and severity of the infection, the chosen herbal remedy, and individual patient factors. Some individuals may experience noticeable improvement within a few days or weeks, while others may require several months of consistent treatment to achieve complete resolution. Patience and adherence to the prescribed treatment regimen are essential.
Question 6: Are there any specific hygiene practices that can enhance the effectiveness of fungus herbal treatment?
Maintaining meticulous hygiene practices is paramount for both preventing and treating fungal infections. This includes regular washing with soap and water, thorough drying of affected areas, wearing breathable clothing and footwear, and avoiding sharing personal items. Proper hygiene creates an unfavorable environment for fungal growth, thereby enhancing the effectiveness of herbal remedies and reducing the risk of recurrence.
These frequently asked questions underscore the importance of informed decision-making, professional guidance, and responsible application when considering botanical remedies for fungal infections.
The following section will explore potential future research directions in the area of fungus herbal treatment.
Fungus Herbal Treatment
This exploration of fungus herbal treatment has highlighted the multifaceted nature of employing botanical remedies to combat fungal infections. It is crucial to acknowledge the significance of accurate fungal identification, judicious herb selection, precise preparation methods, and consistent application, supplemented by meticulous hygiene practices and expert medical guidance. The efficacy of fungus herbal treatment is contingent upon these interrelated factors, underscoring the need for a comprehensive and informed approach.
The potential of fungus herbal treatment lies in its capacity to offer accessible and affordable options, particularly in regions where conventional pharmaceuticals are limited. However, the information presented serves not as a prescription for self-treatment, but as a catalyst for responsible investigation and informed discourse within the medical community. Continued research and rigorous scientific validation remain paramount to establishing the true therapeutic value and safety profile of fungus herbal treatment for the benefit of all.