A traditional approach focusing on natural remedies for managing the symptoms and progression of a chronic lung condition characterized by the irreversible widening of the bronchi. These remedies often include specific plants and their extracts, aimed at reducing inflammation, loosening mucus, and supporting overall respiratory health. As an example, practitioners might employ expectorant herbs to aid in clearing airways, alongside anti-inflammatory herbs intended to reduce bronchial swelling.
Historically, botanical medicine has played a significant role in addressing respiratory ailments, often providing accessible and affordable options, particularly in regions with limited access to conventional medical care. Some proponents suggest that such methods offer a holistic approach, considering the individual’s overall well-being rather than solely targeting the disease itself. Any purported benefits warrant rigorous scientific scrutiny to validate efficacy and safety, as evidence is still being gathered in this field.
The following discussion will explore various botanical substances that have been traditionally used in connection with managing bronchiectasis. It will also examine potential mechanisms of action, current research (or lack thereof), and safety considerations associated with their use. Information presented is for educational purposes and should not be interpreted as medical advice.
Guidance on Complementary Botanical Approaches
The subsequent recommendations offer insights into the responsible and informed consideration of botanical substances in the context of bronchiectasis management. These suggestions are presented for informational purposes and should not supersede the guidance of qualified healthcare professionals.
Tip 1: Prioritize Consultation with Healthcare Providers: Before integrating any botanical substance into a bronchiectasis management plan, a consultation with a physician or qualified respiratory therapist is essential. This ensures the approach is appropriate given individual medical history and current treatments, and to rule out potential interactions.
Tip 2: Investigate the Evidence Base: The scientific evidence supporting the efficacy of various plants and plant-derived compounds in the treatment of bronchiectasis is limited. A thorough literature review is crucial, examining published research studies and meta-analyses when available, to gauge the strength of evidence before making any decisions.
Tip 3: Source Reputable Products: Purity and quality are paramount when selecting any herbal supplement. Prioritize products from established and reputable manufacturers who adhere to rigorous quality control standards. Look for third-party certifications to verify product contents and minimize the risk of contamination.
Tip 4: Be Vigilant for Adverse Effects: As with any therapeutic agent, botanical substances can elicit unwanted side effects or interact with prescribed medications. Closely monitor for any new or worsening symptoms, such as allergic reactions, digestive disturbances, or changes in respiratory function, and report them promptly to a healthcare provider.
Tip 5: Start with Low Doses: When initiating any botanical substance, begin with a low dose and gradually increase it as tolerated, while closely observing for any adverse effects. This minimizes the risk of unexpected reactions and allows for a personalized assessment of efficacy and safety.
Tip 6: Consider Preparatory Methods: The method of preparation can affect the potency and bioavailability of botanical substances. Infusions, decoctions, tinctures, and capsules may have varying effects. Understanding the appropriate preparation method for a specific substance is essential for achieving desired outcomes.
Tip 7: Maintain a Comprehensive Treatment Plan: Botanical substances should be considered as complementary components within a comprehensive bronchiectasis management plan, not as replacements for conventional medical therapies such as bronchodilators, antibiotics, and airway clearance techniques. Adherence to prescribed medications and therapies remains crucial.
These considerations underscore the importance of informed decision-making and responsible integration of botanical substances in managing bronchiectasis, always under the guidance of qualified healthcare professionals.
The next section of this article will delve into specific botanical substances and their applications within the context of supporting respiratory health and managing bronchiectasis symptoms.
1. Symptom alleviation potential
The potential for botanical interventions to alleviate symptoms associated with bronchiectasis represents a primary consideration in the context of herbal strategies. Bronchiectasis manifests with symptoms such as chronic cough, excessive mucus production, shortness of breath, and wheezing. The degree to which herbal remedies can effectively address these symptoms directly influences their perceived value and utility in patient management. For example, certain botanical extracts may possess antitussive properties, potentially reducing the frequency and intensity of cough. The impact on mucus production is equally relevant; substances with mucolytic or expectorant actions could facilitate airway clearance and alleviate associated discomfort. The importance of symptom alleviation is rooted in the immediate enhancement of patient quality of life and functional capacity.
Real-life examples of symptom alleviation potentially attributed to botanical substances include the use of ivy leaf extract for cough relief and eucalyptus oil for its expectorant effects. However, the objective validation of such effects often requires rigorous clinical trials, controlling for placebo effects and confounding variables. The practical significance of understanding symptom alleviation potential lies in the ability to make informed decisions about incorporating herbal remedies into a comprehensive treatment plan. Such decisions must be guided by evidence-based assessments, considering the potential benefits alongside the risks and limitations of each intervention.
In summary, the potential for symptom alleviation represents a central tenet of botanical approaches to bronchiectasis management. The efficacy of these interventions requires meticulous investigation and validation through well-designed studies. Recognizing the limitations of current evidence and prioritizing patient safety are crucial aspects of responsible decision-making. While botanical interventions might offer a complementary approach to symptom management, they should not replace conventional medical therapies without the explicit guidance of a healthcare professional.
2. Mucolytic efficacy examination
The evaluation of mucolytic efficacy holds paramount importance in the sphere of bronchiectasis herbal therapies. The persistent accumulation of viscous mucus in the airways is a hallmark of bronchiectasis, contributing to airway obstruction, recurrent infections, and impaired respiratory function. Therefore, the capacity of herbal interventions to effectively break down and clear this mucus is a critical determinant of their potential therapeutic value.
- Mechanisms of Action
Mucolytic efficacy hinges on disrupting the structural integrity of mucus. This can be achieved through various mechanisms, including the cleavage of disulfide bonds within mucin glycoproteins, the reduction of mucus viscosity by increasing hydration, or the stimulation of ciliary activity to facilitate mucus transport. Herbal substances proposed to possess mucolytic properties may operate via one or more of these pathways. N-acetylcysteine serves as a pharmaceutical example of a mucolytic agent that breaks disulfide bonds, reducing mucus viscosity. Herbal alternatives ideally mimic or enhance natural clearance mechanisms.
- In Vitro and In Vivo Studies
The assessment of mucolytic efficacy typically involves both in vitro and in vivo studies. In vitro studies examine the direct effects of herbal extracts or compounds on mucus samples, measuring parameters such as viscosity, elasticity, and transportability. In vivo studies, often conducted in animal models or clinical trials, evaluate the impact of herbal interventions on mucus clearance in the airways. Results from in vitro experiments need confirmation through in vivo studies. For instance, while an herb may show mucolytic activity in a test tube, it may not translate to actual effectiveness in the human body due to factors like absorption and metabolism.
- Clinical Trial Endpoints
In clinical trials evaluating the mucolytic efficacy of herbal remedies for bronchiectasis, relevant endpoints include changes in sputum volume, sputum viscosity, cough frequency and severity, and measures of pulmonary function, such as forced expiratory volume in one second (FEV1). Subjective patient-reported outcomes, such as perceived ease of breathing and overall symptom burden, are also valuable. Improved sputum clearance, reduced cough, and better breathing, can indicate successful mucolytic action.
- Limitations and Challenges
Evaluating the mucolytic efficacy of herbal interventions poses several challenges. The composition of mucus varies widely among individuals and across different disease states, making it difficult to standardize in vitro testing. Furthermore, the bioavailability and metabolism of herbal compounds can be highly variable, affecting their efficacy in in vivo studies. The lack of standardized methodologies and the potential for placebo effects also complicate the interpretation of clinical trial results. Addressing these limitations requires rigorous study designs, including appropriate control groups, objective outcome measures, and careful consideration of confounding factors.
In summary, the rigorous examination of mucolytic efficacy is essential for determining the potential role of herbal substances in the management of bronchiectasis. A comprehensive assessment involves understanding the mechanisms of action, conducting both in vitro and in vivo studies, defining appropriate clinical trial endpoints, and acknowledging the inherent limitations and challenges associated with evaluating herbal interventions. Only through this rigorous evaluation can the true therapeutic value of herbal mucolytics in the context of bronchiectasis be ascertained.
3. Anti-inflammatory properties research
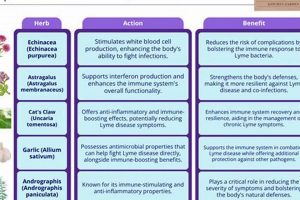
The chronic inflammation characteristic of bronchiectasis contributes significantly to airway damage, mucus hypersecretion, and disease progression. Therefore, anti-inflammatory properties research occupies a central position in evaluating the potential of botanical interventions. The underlying premise is that certain plants contain compounds capable of modulating inflammatory pathways, thereby mitigating the damaging effects of uncontrolled inflammation in the bronchi. This research investigates whether specific herbal extracts can reduce the production of pro-inflammatory cytokines, inhibit the activity of inflammatory enzymes, or promote the resolution of inflammation. The importance stems from the potential to slow disease progression and improve overall respiratory function. For instance, studies might explore the effects of curcumin, derived from turmeric, on reducing neutrophil activity in the airways of bronchiectasis patients. Success in this area would suggest a potential role for turmeric or curcumin supplements in managing the inflammatory component of the disease.
Further analysis involves investigating the specific mechanisms by which herbal compounds exert their anti-inflammatory effects. This often requires detailed biochemical and cellular studies to identify the target molecules and pathways involved. For example, researchers might investigate whether a particular herbal extract inhibits the activation of NF-B, a key transcription factor involved in the expression of pro-inflammatory genes. Practical applications of this research include identifying herbs that can be used as adjunctive therapies to complement conventional treatments for bronchiectasis. The development of standardized herbal formulations with defined anti-inflammatory activity represents another potential outcome. It is essential to note that this research often involves a multidisciplinary approach, combining expertise in botany, pharmacology, immunology, and respiratory medicine.
In conclusion, anti-inflammatory properties research is a critical component of understanding the potential benefits of bronchiectasis herbal approaches. While promising avenues exist, challenges remain in translating preclinical findings into effective clinical therapies. These challenges include the need for well-designed clinical trials, the development of standardized herbal formulations, and the assessment of long-term safety and efficacy. Ongoing research efforts aim to address these challenges and ultimately provide evidence-based options for managing the inflammatory aspects of bronchiectasis using herbal interventions. This research must be viewed as a complementary approach to conventional therapies, not a replacement.
4. Airway protection strategies
In the context of bronchiectasis, compromised airway integrity necessitates focused airway protection strategies. Given the irreversible bronchial dilation that defines the condition, the primary objective shifts to preventing further damage, minimizing infection risk, and preserving remaining lung function. Herbal interventions, therefore, are considered within this framework as potential adjuncts, not replacements, to conventional treatments. These interventions aim to bolster the airways’ natural defenses against irritants and pathogens. Real-life examples include using herbs with purported antioxidant properties to combat oxidative stress within the airways or employing demulcent herbs to soothe irritated bronchial passages. Understanding this connection is significant because it informs a realistic and responsible approach to integrating botanical remedies into a comprehensive management plan.
Further analysis reveals that airway protection strategies within a botanical context encompass multiple facets. One approach involves supporting mucociliary clearance, the lung’s primary mechanism for removing debris and pathogens. Certain herbs are believed to stimulate ciliary beat frequency or alter mucus viscosity, thereby enhancing clearance. Another avenue focuses on modulating the inflammatory response, as chronic inflammation contributes to airway damage. Herbs with anti-inflammatory properties may help to reduce airway edema and prevent further structural deterioration. In practical application, individuals might use a combination of herbal steam inhalations and oral supplements, selected based on their individual needs and under the guidance of a qualified healthcare professional. These applications represent a complementary approach to established medical interventions such as antibiotics, bronchodilators, and airway clearance techniques.
In conclusion, the integration of airway protection strategies within botanical applications for bronchiectasis requires a nuanced understanding of the condition’s pathophysiology and the potential benefits and limitations of herbal interventions. The focus remains on supporting the airways’ natural defenses and preventing further damage. While promising avenues exist, robust clinical evidence is often lacking, underscoring the importance of a cautious and evidence-informed approach. This integration should be viewed as a collaborative effort between the individual, their healthcare providers, and qualified herbal practitioners, with the ultimate goal of improving respiratory health and quality of life.
5. Holistic wellness integration
Holistic wellness integration, in the context of managing bronchiectasis with botanical substances, recognizes the interconnectedness of physical, mental, and emotional well-being. This approach extends beyond merely addressing the immediate symptoms of the condition and aims to foster resilience and optimize overall health, creating an environment conducive to improved respiratory function.
- Lifestyle Modifications
Lifestyle adjustments play a crucial role in holistic wellness integration. Smoking cessation is paramount, as tobacco smoke is a known airway irritant. Regular, moderate exercise, tailored to individual capacity, can enhance lung function and improve overall fitness. Nutritional considerations are also key; a balanced diet rich in antioxidants and anti-inflammatory compounds may support immune function and reduce airway inflammation. Real-life application involves a bronchiectasis patient adopting a personalized exercise routine, quitting smoking, and incorporating antioxidant-rich foods into their daily meals.
- Stress Management Techniques
Chronic stress can exacerbate inflammation and compromise immune function, potentially worsening bronchiectasis symptoms. Stress management techniques, such as mindfulness meditation, yoga, or deep breathing exercises, can help mitigate the negative impacts of stress. These practices promote relaxation, reduce anxiety, and improve overall emotional well-being. A practical example includes a patient engaging in daily mindfulness meditation to manage stress related to their chronic condition, leading to improved sleep and a reduction in cough frequency.
- Sleep Hygiene Optimization
Adequate and restful sleep is essential for immune function and overall health. Poor sleep quality can impair immune responses and increase susceptibility to respiratory infections, a significant concern for individuals with bronchiectasis. Establishing a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment are crucial components of sleep hygiene. An individual with bronchiectasis might implement a regular sleep schedule, avoid caffeine before bed, and create a dark, quiet sleep environment to improve sleep quality.
- Social Support and Emotional Well-being
Strong social connections and a sense of emotional well-being can significantly impact an individual’s ability to cope with a chronic condition like bronchiectasis. Social support provides emotional comfort, reduces feelings of isolation, and promotes adherence to treatment plans. Engaging in activities that bring joy and fulfillment can enhance overall quality of life. A bronchiectasis patient might join a support group to connect with others facing similar challenges, fostering a sense of community and shared understanding, ultimately improving their emotional outlook.
The integration of these facets into a comprehensive management strategy complements botanical interventions by creating a synergistic effect. While botanical substances may address specific symptoms or underlying mechanisms of bronchiectasis, holistic wellness practices enhance the body’s resilience and optimize its capacity to respond to treatment. However, it is essential to recognize that holistic approaches are not a substitute for conventional medical care. Instead, they should be integrated into a comprehensive plan under the guidance of qualified healthcare professionals.
Frequently Asked Questions Regarding Botanical Approaches to Bronchiectasis
The following section addresses common inquiries concerning the utilization of herbal remedies in the context of bronchiectasis management. The information provided is intended for educational purposes and should not be interpreted as medical advice. Consultation with a qualified healthcare professional is essential before initiating any new treatment regimen.
Question 1: Are herbal treatments a cure for bronchiectasis?
No, herbal treatments are not a cure for bronchiectasis. Bronchiectasis is a chronic condition characterized by irreversible airway damage. Botanical interventions may offer symptomatic relief and support overall respiratory health, but they cannot reverse the structural changes associated with the disease.
Question 2: Can herbal remedies replace conventional medical treatments for bronchiectasis?
Herbal remedies should not replace conventional medical treatments for bronchiectasis. Conventional treatments, such as antibiotics, bronchodilators, and airway clearance techniques, are essential for managing infections, improving airflow, and preventing disease progression. Botanical interventions may be used as complementary therapies under the guidance of a healthcare provider.
Question 3: Are herbal treatments for bronchiectasis safe?
The safety of herbal treatments for bronchiectasis varies depending on the specific herb, the dosage, and individual patient factors. Some herbs may interact with medications or cause adverse side effects. It is crucial to consult with a healthcare professional or qualified herbalist to ensure the safety of any herbal regimen.
Question 4: What evidence supports the use of herbal treatments for bronchiectasis?
The evidence supporting the use of herbal treatments for bronchiectasis is limited. Some studies suggest that certain herbs may have anti-inflammatory, mucolytic, or bronchodilator properties, but more rigorous research is needed to confirm these findings. Clinical trials evaluating the efficacy and safety of herbal interventions are often small and of variable quality.
Question 5: How are herbal treatments for bronchiectasis administered?
Herbal treatments for bronchiectasis may be administered in various forms, including teas, tinctures, capsules, and topical applications. The appropriate dosage and method of administration depend on the specific herb, the patient’s individual needs, and the guidance of a healthcare professional or herbalist.
Question 6: Where can individuals find reliable information about herbal treatments for bronchiectasis?
Reliable information about herbal treatments for bronchiectasis can be found through reputable sources, such as scientific journals, medical databases, and websites maintained by healthcare organizations. Consultation with a healthcare professional or qualified herbalist is essential for obtaining personalized and evidence-based guidance.
In summary, botanical approaches may offer a complementary role in managing bronchiectasis symptoms and supporting respiratory health. However, it is crucial to recognize the limitations of current evidence and prioritize patient safety by consulting with qualified healthcare professionals before initiating any new treatment regimen.
The following section will explore potential risks and side effects associated with this approach.
bronchiectasis herbal treatment
The exploration of botanical interventions within the context of bronchiectasis reveals a complex landscape. While certain herbal substances demonstrate potential for symptom alleviation, mucolytic action, and anti-inflammatory effects, the existing evidence base remains limited and often lacks the rigor required for definitive conclusions. Furthermore, concerns regarding safety, standardization, and potential interactions with conventional medications necessitate a cautious and informed approach. The utilization of botanical remedies should not be viewed as a replacement for established medical therapies but rather as a potential adjunct, considered on an individual basis and under the strict supervision of qualified healthcare professionals.
Continued research is crucial to elucidate the true efficacy and safety profiles of specific herbal substances in managing bronchiectasis. Until more robust evidence becomes available, patients and practitioners must prioritize evidence-based medicine, prioritizing treatments with proven benefits while carefully weighing the potential risks and benefits of any complementary approach. The responsible integration of botanical medicine requires ongoing dialogue between patients and healthcare providers, ensuring that decisions are informed, personalized, and aligned with the best available evidence.