Infusions derived from plants, excluding Camellia sinensis, prepared with the intention of alleviating symptoms associated with influenza and the common cold, represent a category of beverages often utilized for their perceived therapeutic properties. These preparations typically involve steeping dried herbs, flowers, roots, or spices in hot water to extract their bioactive compounds. Common ingredients include ginger, chamomile, peppermint, and elderflower, each selected for its purported ability to address specific symptoms such as congestion, sore throat, or fever.
The significance of employing plant-based infusions during periods of illness stems from historical precedent and contemporary research into the pharmacological actions of their constituents. Traditional medicine systems across various cultures have long incorporated these beverages as a primary means of managing upper respiratory infections. The perceived benefits encompass anti-inflammatory, antiviral, and immune-modulatory effects, alongside palliative relief from discomfort. The warm liquid itself can also contribute to hydration and soothing of irritated tissues.
Subsequent sections will delve into specific botanical ingredients commonly incorporated into these remedial infusions, examining the scientific evidence supporting their efficacy, and offering guidelines regarding their safe and appropriate utilization. Furthermore, considerations for individual health conditions and potential interactions with pharmaceutical medications will be addressed.
Guidance on Utilizing Plant-Based Infusions for Influenza and the Common Cold
The following recommendations serve as guidelines for the appropriate and effective utilization of herbal preparations during periods of influenza or the common cold. Individual results may vary, and professional medical advice should always be sought for serious or persistent ailments.
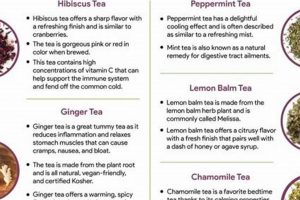
Tip 1: Select Appropriate Ingredients: Opt for botanicals known for their anti-inflammatory, antiviral, or decongestant properties. Ginger, elderflower, peppermint, and eucalyptus are frequently employed. Consult reliable sources for information on the properties of each herb.
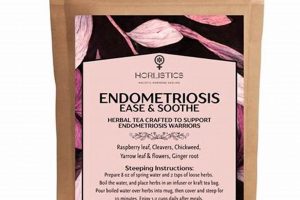
Tip 2: Ensure Proper Preparation: Adhere to recommended steeping times and temperatures for optimal extraction of beneficial compounds. Generally, a steep time of 10-15 minutes in freshly boiled water is sufficient for dried herbs.
Tip 3: Maintain Adequate Hydration: Supplement herbal preparations with sufficient water intake. Hydration is critical for thinning mucus and supporting immune function.
Tip 4: Observe Dosage Guidelines: Avoid excessive consumption of any single herb. Moderation is essential to minimize the risk of adverse effects. Refer to product labels or consult with a qualified herbalist for dosage recommendations.
Tip 5: Monitor for Allergic Reactions: Exercise caution when introducing new herbs into the diet. Discontinue use immediately if signs of an allergic reaction, such as skin rash, itching, or difficulty breathing, develop.
Tip 6: Consider Potential Interactions: Be aware of potential interactions between herbal ingredients and pharmaceutical medications. Consult with a healthcare professional to assess compatibility.
Tip 7: Prioritize Rest and Nutrition: Complement the use of these infusions with adequate rest and a nutrient-rich diet. These supportive measures are crucial for facilitating recovery.
The judicious and informed use of plant-based infusions can serve as a valuable adjunct to conventional medical care in managing the symptoms of influenza and the common cold. However, these preparations should not be considered a substitute for professional medical advice or treatment.
The subsequent section will address potential contraindications and cautionary measures associated with the use of herbal remedies, emphasizing the importance of informed decision-making in healthcare.
1. Symptom alleviation
The primary objective in employing plant-derived infusions during episodes of influenza and the common cold is symptom alleviation. The unpleasant manifestations of these viral infectionsincluding sore throat, nasal congestion, cough, headache, and feversignificantly impact quality of life. Herbal infusions are utilized to mitigate the severity of these symptoms through various mechanisms. For example, infusions containing ginger may reduce nausea and inflammation, thereby indirectly lessening headache severity. Similarly, peppermint infusions can act as a decongestant, easing nasal congestion and facilitating easier breathing. The efficacy of symptom alleviation is frequently assessed through subjective reporting by individuals experiencing these ailments.
The selection of specific herbs for infusion preparation is contingent upon the targeted symptoms. An individual experiencing a sore throat may choose infusions containing chamomile or licorice root, both known for their soothing properties. Conversely, someone suffering from nasal congestion might opt for eucalyptus or peppermint infusions due to their decongestant effects. The preparation method also plays a crucial role; proper steeping ensures optimal extraction of the herb’s active compounds. Inadequate steeping may result in a less potent infusion and, consequently, diminished symptom relief. Real-world examples include individuals using ginger infusions to manage nausea associated with influenza and elderflower infusions to reduce fever. Careful selection and preparation are therefore critical for achieving desired symptomatic outcomes.
The success of symptom alleviation through herbal infusions depends on a multi-faceted approach. Understanding the specific properties of different herbs, proper preparation techniques, and individual patient factors are all critical components. However, it is crucial to acknowledge that these infusions primarily offer symptomatic relief and do not constitute a cure for the underlying viral infection. The challenges lie in standardizing herbal preparations and conducting rigorous clinical trials to definitively establish efficacy and safety. Nevertheless, the understanding that certain herbal infusions can alleviate specific symptoms remains a practically significant and widely adopted approach for managing the discomfort associated with influenza and the common cold.
2. Botanical Properties
The therapeutic potential of infusions intended for the amelioration of influenza and common cold symptoms is intrinsically linked to the inherent botanical properties of the constituent plants. These properties, determined by the plants’ phytochemical composition, dictate the range and intensity of physiological effects elicited upon consumption. A thorough understanding of these properties is paramount for informed and effective utilization.
- Antiviral Activity
Certain plants contain compounds demonstrated to exhibit antiviral activity, interfering with viral replication or attachment. Elderberry (Sambucus nigra), for instance, possesses flavonoids that can inhibit viral entry into host cells. Similarly, licorice root (Glycyrrhiza glabra) contains glycyrrhizin, which exhibits antiviral properties against several viruses. The presence of these compounds in infusions may offer a degree of protection or reduce viral load during infection.
- Anti-Inflammatory Effects
Inflammation is a central component of the immune response to viral infections but can contribute significantly to associated discomfort. Many plants possess anti-inflammatory compounds that can modulate this response. Ginger (Zingiber officinale) contains gingerols and shogaols, which have demonstrated anti-inflammatory properties by inhibiting prostaglandin synthesis. Chamomile (Matricaria chamomilla) contains apigenin, an antioxidant that can reduce inflammation by modulating cytokine production. Infusions prepared with these plants can mitigate inflammation-related symptoms such as sore throat and muscle aches.
- Expectorant and Decongestant Actions
Congestion and mucus production are common symptoms of upper respiratory infections. Certain botanicals exhibit expectorant and decongestant properties, facilitating the clearance of mucus from the respiratory tract. Eucalyptus (Eucalyptus globulus) contains cineole, a compound that thins mucus and acts as a decongestant. Peppermint (Mentha piperita) contains menthol, which has a cooling effect and can help to open airways. Infusions containing these herbs can ease breathing and reduce coughing.
- Immune-Modulating Capabilities
Some plants contain compounds that can modulate the immune system, supporting the body’s natural defenses against infection. Echinacea (Echinacea purpurea) contains polysaccharides and alkylamides that stimulate immune cell activity. Astragalus (Astragalus membranaceus) contains polysaccharides that can enhance immune function by increasing the production of interferon. While the exact mechanisms are complex and not fully understood, the inclusion of these herbs in infusions is thought to bolster immune responses.
The selection of specific botanical ingredients for infusions intended for influenza and common cold symptom management should be guided by a careful consideration of their individual and combined properties. While empirical evidence supports the traditional use of these plants, scientific validation through rigorous clinical trials remains an ongoing area of research. Infusions formulated based on an understanding of botanical properties represent a potential adjunct to conventional medical care, aimed at providing symptomatic relief and supporting the body’s natural healing processes. The appropriate use of plant-based infusions should consider potential drug interactions, individual sensitivities, and should not substitute for professional medical advice.
3. Preparation methods
The efficacy of plant-based infusions in mitigating influenza and common cold symptoms is directly contingent upon meticulous preparation methods. These methods govern the extraction of bioactive compounds from the plant material, thereby influencing the concentration and therapeutic potential of the resulting beverage. Inadequate or inappropriate preparation can significantly diminish the intended benefits, rendering the infusion less effective. Conversely, optimized preparation techniques can maximize the extraction of beneficial phytochemicals, potentially enhancing the infusion’s therapeutic impact.
Key factors influencing preparation efficacy include water temperature, steeping time, and the ratio of herb to water. For instance, excessively high water temperatures can degrade thermolabile compounds, reducing their activity. Insufficient steeping time may result in incomplete extraction, leaving potentially beneficial compounds within the plant material. An inadequate herb-to-water ratio may lead to a weak infusion lacking sufficient concentration of active constituents. A real-world example is observed when preparing ginger infusions. Using boiling water can destroy some of ginger’s volatile oils, reducing its anti-inflammatory effects. A more effective approach is to use simmering water (around 80C) and a steeping time of 10-15 minutes. Furthermore, the form of the herb, whether fresh, dried, or powdered, also affects the extraction process. Finely ground herbs generally release their compounds more readily than coarsely chopped or whole herbs. The choice of container material (glass, ceramic, or metal) can also subtly impact the infusion, although this effect is typically less pronounced than other variables. It is also vital to consider the possible contaminants of water before the preparation of infusions.
In summary, the preparation methods employed in creating plant-based infusions for influenza and the common cold are not merely procedural steps, but critical determinants of therapeutic outcome. An understanding of these methods, encompassing temperature control, steeping duration, herb-to-water ratios, and herb form, is essential for maximizing the potential benefits of these traditional remedies. The challenge lies in establishing standardized preparation protocols for various herbal infusions and disseminating this knowledge effectively to ensure consistent and reliable results. However, until comprehensive standardization is achieved, a mindful and informed approach to preparation remains paramount for harnessing the therapeutic potential of plant-based infusions. Finally, remember to clean the kitchen utensils to prepare your herbal tea infusions.
4. Hydration support
Adequate fluid intake constitutes a cornerstone of supportive care during episodes of influenza and the common cold. The physiological demands imposed by these infections necessitate increased hydration to counteract fluid losses and facilitate optimal bodily function. Plant-based infusions, while offering potential therapeutic benefits, also serve as a valuable source of hydration, contributing to overall wellness during illness.
- Counteracting Dehydration
Fever, a common symptom of influenza, elevates metabolic rate and increases insensible fluid losses through perspiration. Similarly, gastrointestinal symptoms such as vomiting or diarrhea, which can accompany viral infections, further exacerbate fluid depletion. Plant-based infusions, consumed regularly, help replenish these lost fluids, mitigating the risk of dehydration and its associated complications, such as headache, fatigue, and impaired cognitive function. For example, consistent sipping of warm herbal infusions throughout the day aids in maintaining fluid balance and preventing dehydration.
- Mucus Thinning and Expectorant Action
Respiratory tract infections often result in increased mucus production, contributing to congestion and coughing. Adequate hydration, facilitated by the consumption of plant-based infusions, promotes the thinning of mucus, making it easier to expel. This expectorant action can alleviate respiratory distress and reduce the duration of coughing episodes. The warm liquid itself soothes irritated respiratory passages, further enhancing this effect. A real-world instance is drinking peppermint tea that helps loosen congestion and facilitates easier breathing.
- Facilitating Renal Function
Maintaining adequate hydration is essential for optimal renal function, enabling the kidneys to efficiently filter waste products and toxins from the bloodstream. During infections, metabolic waste production may increase, placing a greater burden on the kidneys. Plant-based infusions, contributing to overall fluid intake, support renal function and prevent the accumulation of toxins. Regular consumption assists the body’s natural detoxification processes and reduces the risk of complications.
- Enhancing Medication Efficacy
Hydration can indirectly influence the efficacy of certain medications used to treat influenza and the common cold. Adequate fluid intake promotes optimal absorption and distribution of medications, ensuring they reach their intended target tissues effectively. Dehydration, conversely, can impair drug absorption and reduce their therapeutic effect. For instance, drinking herbal tea with acetaminophen can support its absorption and help reduce fever effectively.
In summary, the role of hydration support in managing influenza and the common cold extends beyond simple fluid replacement. Plant-based infusions, by providing a palatable and potentially therapeutic source of hydration, contribute to multiple physiological processes essential for recovery. These benefits, encompassing dehydration prevention, mucus thinning, renal function support, and medication efficacy enhancement, underscore the importance of prioritizing adequate fluid intake during these illnesses. Furthermore, infusions can be combined with honey and lemon to enhance hydration and further alleviate symptoms.
5. Safety considerations
The intersection of safety considerations and plant-based infusions intended for influenza and the common cold necessitates careful evaluation. While perceived as natural and benign, herbal remedies are not inherently without risk. The ingestion of such infusions can precipitate adverse reactions, interact with pharmaceutical medications, or exacerbate pre-existing medical conditions. The absence of standardized regulation and quality control in the herbal product industry further compounds these concerns. Therefore, a comprehensive understanding of potential hazards and appropriate mitigation strategies is essential for responsible utilization. The consumption of St. John’s Wort, often marketed as an immune booster, can interact negatively with certain antidepressants, reducing their effectiveness. This illustrates the importance of awareness regarding herb-drug interactions.
Several factors contribute to the potential for adverse effects associated with plant-based infusions. Herb-drug interactions represent a significant concern, particularly for individuals concurrently taking prescription medications. Certain herbal constituents can inhibit or induce hepatic enzymes responsible for drug metabolism, altering drug concentrations and potentially leading to toxicity or therapeutic failure. Allergic reactions to herbal ingredients are also a possibility, ranging from mild skin rashes to severe anaphylaxis. Additionally, the presence of contaminants, such as heavy metals or pesticides, in herbal products poses a risk to consumer health. Quality control measures, including sourcing from reputable suppliers and verifying product purity, are crucial in minimizing this risk. For example, pregnant women should exercise extreme caution when consuming herbal infusions, as some ingredients can have teratogenic effects.
In conclusion, the safe and responsible utilization of plant-based infusions for influenza and the common cold requires a proactive approach to risk assessment and mitigation. Awareness of potential herb-drug interactions, allergic sensitivities, and product quality concerns is paramount. Consultation with a qualified healthcare professional, including a physician or experienced herbalist, is recommended prior to incorporating these remedies into a treatment plan, particularly for individuals with pre-existing medical conditions or those taking prescription medications. Although, there are herbal teas that are generally considered safe for consumption such as ginger and chamomile.
6. Potential interactions
The concurrent consumption of herbal infusions and pharmaceutical medications necessitates a rigorous evaluation of potential interactions, a critical aspect of safety when utilizing plant-based remedies during influenza and the common cold. Such interactions can compromise the efficacy of prescribed treatments or potentiate adverse effects, thereby impacting patient outcomes.
- Cytochrome P450 Modulation
Many herbal constituents possess the capacity to either inhibit or induce cytochrome P450 (CYP) enzymes, a family of hepatic enzymes responsible for metabolizing a significant proportion of pharmaceutical drugs. Inhibition of CYP enzymes can lead to elevated drug concentrations, increasing the risk of toxicity. Conversely, induction can accelerate drug metabolism, reducing therapeutic efficacy. For example, St. John’s Wort (Hypericum perforatum), often consumed for its purported mood-boosting properties, is a potent CYP3A4 inducer and can decrease the effectiveness of oral contraceptives, anticoagulants, and certain immunosuppressants. It is important to consider its interactions with herbal tea such as ginger or chamomile for cold and flu.
- Pharmacodynamic Synergism or Antagonism
Herbal infusions may exhibit synergistic or antagonistic effects when combined with medications acting on similar physiological pathways. For instance, the concurrent use of chamomile, known for its sedative properties, with benzodiazepines or other central nervous system depressants can potentiate drowsiness and increase the risk of respiratory depression. Conversely, the consumption of herbs with diuretic effects alongside prescription diuretics can lead to excessive fluid loss and electrolyte imbalances. These combined effects are crucial to consider when integrating such infusions during a cold and flu treatment.
- Absorption Interference
Certain herbal constituents can interfere with the absorption of pharmaceutical drugs in the gastrointestinal tract. Tannins, present in some herbal teas, can bind to metal ions and impair the absorption of iron supplements or certain antibiotics. Mucilage-containing herbs, such as slippery elm, can form a physical barrier in the gut, hindering the absorption of medications taken concurrently. To mitigate this risk, it is generally recommended to separate the administration of herbal infusions and pharmaceutical drugs by at least two hours. The interaction of slippery elm should be considered if an herbal tea for cold and flu contains this substance.
- Effects on Blood Clotting
Several herbs possess anticoagulant or antiplatelet properties, potentially increasing the risk of bleeding when combined with anticoagulant medications such as warfarin or antiplatelet drugs such as aspirin. Ginger, garlic, and Ginkgo biloba are examples of herbs with known effects on blood clotting. The concurrent use of these herbs with anticoagulants necessitates careful monitoring of coagulation parameters and should be undertaken only under the supervision of a healthcare professional. Consumption of herbal teas with such anticoagulant elements for cold and flu symptoms, coupled with blood-thinning drugs can be detrimental.
These examples underscore the critical importance of considering potential interactions when using herbal infusions for influenza and the common cold, particularly in individuals taking pharmaceutical medications. A comprehensive medication history, including both prescription and over-the-counter drugs, as well as herbal supplements, is essential for healthcare professionals to assess the risk of interactions and provide appropriate guidance. The development of reliable resources providing evidence-based information on herb-drug interactions is crucial for promoting safe and effective use of herbal remedies. Thus, care should be taken to check the ingredients in herbal tea, with your existing medications, for any dangerous reactions when planning to treat cold and flu symptoms.
7. Rest and Nutrition
Adequate rest and appropriate nutrition are integral components of a holistic approach to managing influenza and the common cold, acting synergistically with the potential benefits derived from plant-based infusions. While herbal teas can offer symptomatic relief through various mechanisms, their effectiveness is amplified when coupled with sufficient rest and a diet that supports immune function. The body’s capacity to combat viral infections is significantly compromised in states of sleep deprivation and nutritional deficiency, thereby diminishing the potential impact of any adjunctive therapies, including herbal remedies. For example, an individual consuming ginger tea to alleviate nausea but simultaneously engaging in strenuous activity and neglecting dietary intake will likely experience diminished symptom relief and a prolonged recovery period.
Rest facilitates the conservation of energy, allowing the immune system to dedicate its resources towards fighting the infection. During sleep, the body releases cytokines, proteins that help regulate immune responses. Conversely, sleep deprivation can suppress immune function, making the individual more susceptible to secondary infections. A nutrient-rich diet provides the essential building blocks for immune cells and supports the production of antibodies. Vitamin C, zinc, and protein are particularly important for immune function. For instance, incorporating citrus fruits, lean meats, and leafy green vegetables into the diet alongside the consumption of elderberry tea can enhance immune responses and potentially shorten the duration of the illness. Furthermore, avoiding processed foods, sugary drinks, and excessive alcohol consumption minimizes inflammation and further supports immune function. Prioritization of these measures provides additional support to the benefits provided by herbal treatments.
In conclusion, the use of plant-based infusions for influenza and the common cold should not be viewed in isolation but rather as part of a comprehensive strategy that prioritizes both rest and nutrition. These fundamental elements provide the necessary foundation for optimal immune function, enhancing the potential benefits of herbal remedies and facilitating a more rapid and complete recovery. The challenge lies in promoting widespread awareness of the interconnectedness of these factors and encouraging individuals to adopt a holistic approach to managing these common illnesses. Recognizing and promoting the interaction between healthy habits with the consumption of infusions offers additional patient support.
Frequently Asked Questions Regarding Herbal Infusions for Influenza and the Common Cold
The following questions address common inquiries and misconceptions concerning the use of plant-based infusions as a supportive measure during episodes of influenza and the common cold. The information presented aims to provide clarity and promote informed decision-making.
Question 1: Are herbal infusions a substitute for conventional medical treatment for influenza and the common cold?
Herbal infusions are not a substitute for conventional medical treatment. They should be considered a complementary approach aimed at alleviating symptoms. Individuals experiencing severe or persistent symptoms should seek professional medical advice and treatment.
Question 2: Is there scientific evidence to support the efficacy of herbal infusions for influenza and the common cold?
Some herbal ingredients have demonstrated antiviral, anti-inflammatory, or decongestant properties in laboratory studies. However, rigorous clinical trials evaluating the efficacy of specific herbal infusions for influenza and the common cold are limited. Evidence is often derived from traditional use and anecdotal reports.
Question 3: Are herbal infusions safe for everyone?
Herbal infusions may not be safe for everyone. Individuals with allergies to specific plants, pregnant or breastfeeding women, and those taking certain medications should exercise caution and consult with a healthcare professional before use. Potential herb-drug interactions and contraindications exist.
Question 4: How should herbal infusions be prepared for optimal benefit?
Proper preparation is crucial for maximizing the extraction of beneficial compounds. Generally, dried herbs should be steeped in freshly boiled water for 10-15 minutes. The specific steeping time and temperature may vary depending on the herb. Adhering to recommended guidelines is essential.
Question 5: Can herbal infusions prevent influenza and the common cold?
There is no conclusive evidence to suggest that herbal infusions can prevent influenza or the common cold. While some herbs may possess immune-modulating properties, they are not a substitute for vaccination or other preventative measures such as frequent handwashing.
Question 6: Are all herbal products of equal quality?
No, herbal product quality can vary significantly. It is important to source herbal products from reputable suppliers who adhere to quality control standards. Look for products that have been tested for purity and potency.
In summary, herbal infusions can offer a supportive role in managing symptoms associated with influenza and the common cold, but they should not replace conventional medical care. Informed decision-making, guided by an understanding of potential risks and benefits, is paramount.
The subsequent section will provide a concluding summary of the key points discussed throughout this discourse, emphasizing the importance of responsible and informed utilization of plant-based remedies.
Conclusion
This exploration of herbal tea for flu and cold has illuminated key aspects surrounding its use as a supportive measure. The discussion has encompassed symptom alleviation, botanical properties, preparation methods, hydration support, safety considerations, potential interactions with medications, and the importance of rest and nutrition. It is evident that the judicious and informed application of these plant-derived infusions may contribute to managing the discomfort associated with these common viral infections.
The ongoing pursuit of scientific validation through rigorous research remains essential for establishing definitive efficacy and safety profiles. As knowledge evolves, the responsible integration of herbal tea for flu and cold into holistic healthcare strategies necessitates continuous evaluation and a commitment to evidence-based practices. The informed consumer, armed with a critical understanding of both potential benefits and risks, is best positioned to make judicious choices in the management of personal health.