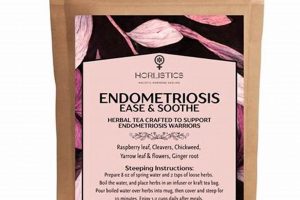
A beverage crafted from a blend of various herbs, traditionally consumed to support lactation and maternal well-being during the postpartum period. These formulations often include ingredients such as fennel, fenugreek, blessed thistle, and chamomile, each selected for properties believed to promote milk production and soothe both mother and child. The specific composition can vary significantly based on regional traditions and individual needs.
The significance of these herbal preparations lies in their potential to provide natural support during a crucial time for both mother and infant. Historically, many cultures have relied on botanical remedies to aid lactation. Proponents suggest benefits including increased milk supply, reduced colic in infants through the mother’s consumption, and calming effects for both the mother and child. However, it is imperative to acknowledge that the efficacy of specific formulations is subject to ongoing scientific investigation, and individual responses can differ substantially.
The following sections will explore aspects of herbal galactagogues, including specific herbal ingredients commonly found in these formulations, potential risks and benefits associated with their use, guidelines for responsible consumption, and critical considerations for consulting with healthcare professionals before incorporating them into a postpartum care regimen.
Guidelines for Thoughtful Consumption
The following recommendations provide considerations when deciding to incorporate an herbal lactation beverage into a postpartum routine. Prioritize informed choices and professional guidance.
Tip 1: Consult a Healthcare Provider. Before introducing any new substance into the diet, particularly while breastfeeding, a consultation with a physician, lactation consultant, or qualified herbalist is paramount. Individual health conditions, allergies, and potential interactions with existing medications must be evaluated.
Tip 2: Research Ingredient Safety Profiles. Each herb possesses a unique profile of potential benefits and risks. Conduct thorough research on the safety of individual components, paying close attention to contraindications, potential allergens, and known side effects for both mother and infant.
Tip 3: Begin with a Conservative Approach. When initiating consumption, start with small quantities to assess individual tolerance. Monitor both maternal and infant responses for any adverse reactions, such as digestive upset, skin rashes, or changes in infant behavior.
Tip 4: Prioritize Quality and Source Transparency. Select products from reputable sources that adhere to rigorous quality control standards. Opt for organic or wildcrafted herbs to minimize potential exposure to pesticides and contaminants. Verify ingredient sourcing and manufacturing processes.
Tip 5: Consider Potential Drug Interactions. Certain herbs can interact with pharmaceutical medications. Disclose all medications and supplements currently being taken to a healthcare provider to prevent adverse interactions.
Tip 6: Monitor Milk Supply and Infant Weight Gain. Track milk production and infant weight gain to objectively assess the efficacy of the preparation. If concerns arise, reassess the appropriateness of the formulation with a healthcare professional.
Tip 7: Be Mindful of Allergenic Potential. Many herbs are known allergens. Exercise caution, particularly if there is a family history of allergies, and monitor for any signs of allergic reactions in both the mother and infant.
Adhering to these guidelines can assist in promoting a safe and informed approach to utilizing herbal lactation support. Individual needs and responses vary, emphasizing the importance of professional medical guidance.
The subsequent section will delve into potential benefits, contraindications, and further critical considerations for informed usage.
1. Lactation Support
Lactation support encompasses a range of interventions and practices aimed at optimizing breastfeeding outcomes for both mother and infant. Herbal nursing teas, as a subset of lactation support strategies, have been employed across cultures, positing benefits through the purported galactagogue properties of their constituent herbs. The intersection between lactation support and these herbal preparations warrants careful examination, considering both potential advantages and inherent limitations.
- Hormonal Influence
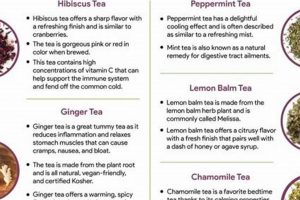
Certain herbs present in nursing teas, such as fenugreek and fennel, contain compounds that may influence hormonal pathways involved in milk production. These compounds are theorized to stimulate prolactin release, a key hormone regulating lactation. While anecdotal evidence and some studies suggest a positive correlation, the extent of hormonal influence and its consistency across individuals require further investigation.
- Hydration and Fluid Intake
Adequate hydration is essential for optimal milk production. The consumption of herbal teas contributes to overall fluid intake, potentially supporting lactation through this mechanism. However, it is crucial to recognize that the benefits derived from increased hydration can be achieved through the consumption of plain water or other non-herbal beverages. The specific contribution of the herbal components beyond hydration remains a point of consideration.
- Soothing and Relaxation Effects
Stress and anxiety can negatively impact milk production. Certain herbs, such as chamomile and lemon balm, are traditionally used for their calming properties. These ingredients in nursing teas may promote relaxation, indirectly supporting lactation by mitigating stress-related inhibition of milk release. The subjective nature of these effects necessitates caution in attributing direct galactagogue properties solely to the calming herbs.
- Placebo Effect
The belief in the efficacy of a treatment can influence its perceived outcome. The act of consuming a beverage specifically intended to enhance lactation may elicit a placebo effect, leading to a perceived increase in milk production or a heightened sense of well-being. This psychological aspect should be considered when evaluating the effectiveness of herbal nursing teas, as it can contribute to reported benefits independently of any direct physiological effects of the herbs themselves.
In summary, the connection between lactation support and herbal nursing teas involves a complex interplay of hormonal, physiological, and psychological factors. While these herbal preparations may offer benefits in certain cases, a critical and evidence-based approach is necessary. Furthermore, individualized assessment and consultation with healthcare professionals remain paramount to ensuring the safety and efficacy of any lactation support strategy.
2. Herbal Galactagogues
Herbal galactagogues represent a category of botanicals traditionally used to promote or increase breast milk production. Herbal nursing tea often incorporates these galactagogues as its active ingredients. The direct connection is that the selection and concentration of these herbs within the tea formulation determine its intended effect on lactation. For example, teas containing fenugreek are predicated on the belief that compounds within the seed stimulate milk-producing hormones. The effectiveness of a given tea is directly tied to the presence and bioavailability of these compounds.
The importance of understanding herbal galactagogues as a component of nursing tea lies in the potential for both benefit and risk. While some mothers experience increased milk supply, others may not, or may experience adverse reactions. For instance, high doses of fenugreek can, in some cases, cause gastrointestinal upset in both mother and infant. Blessed thistle is another commonly included galactagogue, but scientific evidence supporting its efficacy remains limited. Therefore, it is critical to appreciate that the composition of herbal nursing tea is not uniform, and its effects are contingent on the specific galactagogues included and their individual actions.
In conclusion, the relationship between herbal galactagogues and herbal nursing tea is fundamental. The tea serves as a delivery mechanism for the galactagogues, and the intended effects of the tea are reliant on the properties of the incorporated herbs. However, it is equally essential to recognize that efficacy and safety depend on the specific herbal composition, proper dosage, and individual response. A knowledgeable approach, ideally guided by a healthcare professional, is necessary to navigate the potential benefits and risks associated with these herbal preparations.
3. Maternal Wellness
Maternal wellness encompasses the physical, emotional, and psychological well-being of a woman during pregnancy, childbirth, and the postpartum period. It is a multifaceted construct intricately linked to successful breastfeeding outcomes, and, by extension, the use of herbal preparations intended to support lactation. The perceived benefits and risks of incorporating herbal nursing tea into a postpartum regimen must be evaluated within the broader context of maternal well-being.
- Stress Reduction and Relaxation
The postpartum period is frequently characterized by significant stress, sleep deprivation, and emotional fluctuations. Certain herbs commonly found in nursing teas, such as chamomile and lavender, are traditionally used for their calming and anxiolytic properties. If these teas contribute to reduced stress levels and improved relaxation, this may indirectly support maternal well-being and, consequently, potentially enhance lactation. However, it is essential to recognize that the efficacy of these herbs in alleviating postpartum stress may vary among individuals, and they should not be considered a substitute for professional mental health support when necessary.
- Nutritional Support and Hydration
Maintaining adequate nutrition and hydration is crucial for postpartum recovery and milk production. Herbal nursing teas can contribute to fluid intake, providing a source of hydration beyond plain water. Furthermore, some herbal ingredients may offer nutritional benefits, such as vitamins and minerals. However, it is vital to ensure that the tea is not used as a replacement for a balanced and nutritious diet. The primary focus should remain on consuming a variety of whole foods to meet the increased nutritional demands of the postpartum period.
- Cultural and Social Context
The use of herbal remedies during the postpartum period is often deeply rooted in cultural traditions and social practices. In many societies, the consumption of specific herbal teas is a customary way to support maternal health and breastfeeding. These practices can provide a sense of connection to cultural heritage and a feeling of social support, both of which contribute to overall maternal well-being. However, it is important to critically evaluate traditional practices to ensure that they are safe and evidence-based, rather than relying solely on anecdotal evidence.
- Perceived Self-Efficacy and Empowerment
The act of taking proactive steps to support lactation, such as consuming herbal nursing tea, may contribute to a mother’s sense of self-efficacy and empowerment. Feeling in control of one’s breastfeeding journey can enhance maternal confidence and reduce anxiety. However, it is crucial to avoid creating a situation where mothers feel pressured to use herbal remedies or experience guilt if they choose not to. The emphasis should be on providing informed choices and respecting individual preferences.
In conclusion, the connection between maternal wellness and herbal nursing tea is complex and multifaceted. While these herbal preparations may offer potential benefits in terms of stress reduction, nutritional support, cultural connection, and perceived self-efficacy, they should be used judiciously and in conjunction with other essential aspects of postpartum care, including adequate nutrition, hydration, rest, and social support. Moreover, consulting with healthcare professionals is crucial to ensure the safety and appropriateness of herbal remedies for individual circumstances.
4. Infant Safety
Infant safety constitutes a primary concern when considering the maternal consumption of herbal nursing tea. The infant’s exposure to herbal constituents occurs primarily through breast milk, necessitating a thorough understanding of potential effects. Certain herbs, while considered safe for adults in moderate amounts, may pose risks to infants due to their immature metabolic systems and heightened sensitivity. For example, some herbs can induce gastrointestinal distress, allergic reactions, or, in rare cases, more serious adverse events in infants. Therefore, the composition and concentration of herbs within the tea necessitate careful scrutiny before maternal consumption. The selection of herbs for a nursing tea should prioritize those with well-established safety profiles for infants, and the quantities consumed should remain within conservative limits.
Real-world examples illustrate the importance of considering infant safety. Reports of colic-like symptoms, excessive crying, or changes in sleep patterns following maternal consumption of herbal teas underscore the potential for adverse effects. Conversely, anecdotal evidence suggests that certain herbs, such as chamomile, may promote calmness in infants through breast milk transmission; however, such claims warrant scientific validation. Manufacturers and consumers alike share a responsibility to ensure product safety and transparency. Clear labeling of ingredients, including potential allergens, and provision of information on safe usage guidelines are crucial steps. Furthermore, healthcare professionals, including pediatricians and lactation consultants, play a vital role in providing guidance to mothers regarding the use of herbal nursing teas, considering individual infant health factors.
In conclusion, infant safety is paramount in the context of herbal nursing tea. A cautious and informed approach is essential to minimize potential risks. The responsibility for ensuring infant safety rests with manufacturers, healthcare providers, and breastfeeding mothers. By prioritizing ingredient transparency, adhering to recommended dosages, and monitoring infants for any adverse reactions, the potential benefits of herbal nursing teas can be realized while safeguarding infant well-being. Further research into the safety profiles of specific herbs for infants is warranted to strengthen evidence-based recommendations and enhance consumer confidence.
5. Quality Sourcing
The quality of the herbs used in herbal nursing tea directly impacts its safety, efficacy, and overall value. Quality sourcing, therefore, is not merely a desirable attribute but a critical determinant of the product’s integrity. The cause-and-effect relationship is straightforward: inferior sourcing introduces contaminants, reduces potency, and jeopardizes consumer health. For example, herbs grown in polluted environments may accumulate heavy metals, negating any potential benefit and introducing a serious health hazard. Similarly, misidentified or adulterated herbs can lead to unintended and potentially harmful effects, especially for vulnerable populations like breastfeeding mothers and their infants.
The importance of quality sourcing is further underscored by the absence of stringent regulatory oversight in some herbal supplement markets. This necessitates that manufacturers and consumers alike prioritize transparency and traceability. Certifications such as organic or Good Manufacturing Practices (GMP) can provide some assurance, but ultimately, a comprehensive understanding of the supply chain is essential. Real-life instances of herbal supplement contamination, such as the presence of undeclared pharmaceuticals or high levels of pesticides, highlight the dire consequences of neglecting quality sourcing. Selecting reputable brands that conduct thorough testing and provide detailed information about their sourcing practices is a practical application of this understanding. This might involve examining the company’s website, reviewing third-party lab reports, and contacting the manufacturer directly with inquiries.
In conclusion, quality sourcing is an indispensable component of herbal nursing tea. Its absence undermines the very purpose of the product and poses significant risks to both mother and infant. The challenges in ensuring quality necessitate a proactive and informed approach, emphasizing transparency, traceability, and independent verification. A heightened awareness of sourcing practices and a commitment to selecting reputable products are crucial steps in safeguarding the health and well-being of breastfeeding mothers and their children.
6. Professional Guidance
The incorporation of herbal nursing tea into a postpartum regimen necessitates careful consideration, especially given the potential for variability in individual responses and the inherent complexity of herbal interactions. Professional guidance provides a critical safeguard, ensuring that decisions regarding the use of such teas are informed, individualized, and aligned with best practices.
- Assessment of Individual Health History
Healthcare providers possess the expertise to evaluate an individual’s medical history, including allergies, existing medical conditions, and current medications. This assessment is crucial in identifying potential contraindications or interactions with the herbal components of the tea. For example, individuals with certain autoimmune disorders may need to avoid specific herbs known to stimulate the immune system. A lactation consultant can also assess milk supply issues to determine if herbal galactagogues are appropriate or if other interventions are more suitable.
- Informed Decision-Making
Professional guidance empowers individuals to make informed decisions about the use of herbal nursing tea by providing access to evidence-based information. This includes understanding the potential benefits and risks associated with specific herbal ingredients, as well as the limitations of available scientific evidence. Healthcare providers can also dispel misconceptions and address concerns, promoting a balanced and realistic perspective. For instance, a physician can explain that while fenugreek is commonly used to increase milk supply, its effectiveness is not guaranteed, and it may cause side effects in some individuals.
- Dosage and Monitoring
Determining the appropriate dosage of herbal nursing tea is essential to maximize potential benefits while minimizing the risk of adverse effects. Healthcare providers can provide guidance on dosage based on individual factors such as body weight, health status, and milk supply needs. Furthermore, they can monitor the mother and infant for any signs of adverse reactions, such as gastrointestinal distress, skin rashes, or changes in infant behavior. This monitoring allows for timely adjustments in dosage or discontinuation of the tea if necessary. A registered dietitian, for example, could advise on optimal timing for tea consumption relative to meals and breastfeeding sessions.
- Integration with Comprehensive Care
Professional guidance ensures that the use of herbal nursing tea is integrated into a comprehensive postpartum care plan. This may include recommendations for proper nutrition, hydration, rest, and stress management. Healthcare providers can also provide referrals to other specialists, such as lactation consultants, mental health professionals, or registered dietitians, to address specific needs. This holistic approach recognizes that lactation support is not solely dependent on herbal interventions but requires a multi-faceted strategy. For example, a psychologist may offer techniques to reduce stress, which in turn can positively impact milk production, complementing the potential effects of the tea.
In summary, professional guidance is indispensable for the safe and effective use of herbal nursing tea. By providing individualized assessments, evidence-based information, dosage recommendations, monitoring, and integration with comprehensive care, healthcare providers empower individuals to make informed choices that promote maternal and infant well-being. This proactive approach maximizes the potential benefits of herbal nursing tea while mitigating potential risks.
Frequently Asked Questions
The following questions address common concerns and misconceptions surrounding the use of herbal nursing tea. The information provided is intended for educational purposes and should not be considered a substitute for professional medical advice.
Question 1: What constitutes “herbal nursing tea” and what is its intended purpose?
Herbal nursing tea is a beverage formulated from various herbs believed to possess galactagogue properties, meaning they may promote or increase breast milk production. The intended purpose is to provide natural support for lactation during the postpartum period.
Question 2: Are all herbal nursing teas equally effective?
No. The effectiveness of a specific herbal nursing tea depends on several factors, including the types and concentrations of herbs used, the quality of the ingredients, and individual physiological responses. Formulations vary considerably, and efficacy is not guaranteed.
Question 3: What are the potential risks associated with consuming herbal nursing tea?
Potential risks include allergic reactions, gastrointestinal upset in both mother and infant, interactions with medications, and the presence of contaminants if the herbs are not sourced properly. Certain herbs may be contraindicated for individuals with specific medical conditions.
Question 4: Is there scientific evidence to support the claims made about herbal nursing tea?
The scientific evidence supporting the efficacy of many herbal galactagogues is limited and often based on small-scale studies or anecdotal evidence. Some herbs have shown promising results in research, while others lack sufficient evidence to support their use. More rigorous research is needed to determine the true effectiveness of various herbal formulations.
Question 5: How should herbal nursing tea be incorporated into a postpartum care plan?
Herbal nursing tea should be considered as one component of a comprehensive postpartum care plan that includes adequate nutrition, hydration, rest, and stress management. It should not be used as a substitute for professional medical advice or treatment. Consultation with a healthcare provider or lactation consultant is recommended before initiating use.
Question 6: Where can reliable information about herbal nursing tea be obtained?
Reliable information can be obtained from healthcare providers, lactation consultants, registered dietitians, and reputable sources such as peer-reviewed scientific journals and evidence-based websites. Be wary of unsubstantiated claims or testimonials.
Key takeaways from this FAQ section include the importance of individual assessment, evidence-based decision-making, and professional guidance when considering the use of herbal nursing tea. Safety and efficacy are paramount considerations.
The subsequent section will provide a concise summary of the key points discussed in this exploration of herbal nursing tea.
Herbal Nursing Tea
This exploration of herbal nursing tea has revealed a complex landscape of potential benefits, inherent risks, and critical considerations. While these herbal preparations are often sought for their purported galactagogue properties, the scientific evidence supporting their efficacy remains variable. Maternal and infant safety must be prioritized, necessitating careful attention to ingredient sourcing, dosage guidelines, and individual responses. The importance of professional guidance from healthcare providers cannot be overstated, as it facilitates informed decision-making and ensures integration with comprehensive postpartum care.
The utilization of herbal nursing tea, therefore, should not be approached as a panacea, but rather as a potential adjunct to evidence-based lactation support strategies. Further research is warranted to elucidate the specific mechanisms of action of various herbal galactagogues and to establish robust safety profiles for both mothers and infants. Until such data are available, a cautious and informed approach, guided by professional expertise, remains paramount to maximizing potential benefits while minimizing potential harm.