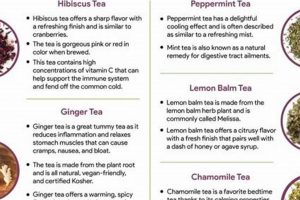
Infusions derived from various plants have been used traditionally to alleviate symptoms associated with hypersensitivity reactions. These preparations, often consumed as beverages, incorporate botanicals believed to possess properties that can modulate the body’s response to allergens. Examples include nettle leaf, known for its potential anti-inflammatory effects, and rooibos, which contains antioxidants that may help stabilize mast cells.
The historical context of utilizing plant-based remedies for managing allergic responses dates back centuries across numerous cultures. Such practices highlight the long-standing recognition of the potential of natural substances to support the body’s defense mechanisms. Benefits may include reducing inflammation, supporting the immune system, and providing symptomatic relief from common allergic manifestations, offering a complementary approach to conventional treatments.
The following sections will delve into specific types of these botanical infusions, examining their purported mechanisms of action, relevant scientific evidence, and potential considerations for their use in managing allergic conditions. This exploration seeks to provide a balanced perspective on their role in promoting well-being and symptom management.
Guidance on Employing Botanical Infusions for Hypersensitivity Mitigation
The following guidelines are presented to assist in the informed consideration of plant-derived beverages as a complementary approach to allergy management.
Tip 1: Source Selection: Prioritize reputable suppliers known for rigorous quality control and accurate botanical identification. This minimizes the risk of contamination or adulteration, ensuring the intended therapeutic compounds are present.
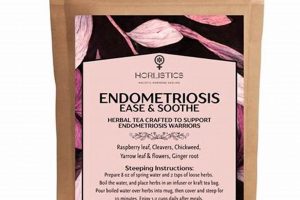
Tip 2: Adherence to Brewing Protocols: Follow recommended steeping times and water temperatures for each specific botanical. Deviation may compromise the extraction of active constituents, diminishing the potential efficacy.
Tip 3: Incremental Introduction: Begin with small quantities to assess individual tolerance and potential adverse reactions. Monitor for any signs of allergic response or gastrointestinal distress.
Tip 4: Awareness of Potential Interactions: Consult a healthcare professional regarding potential interactions with existing medications or pre-existing health conditions. Certain botanicals may potentiate or diminish the effects of pharmaceutical interventions.
Tip 5: Sustained and Consistent Consumption: A single instance of consumption is unlikely to yield significant results. Consistent, long-term integration into a daily routine may be necessary to observe noticeable benefits.
Tip 6: Complementary Role: These infusions should not be considered a replacement for conventional medical treatment for allergies. They serve as a supplementary measure to potentially alleviate symptoms and support overall well-being.
Tip 7: Understanding Limitations: Recognize that the scientific evidence supporting the efficacy of specific botanicals for allergy relief may be limited or preliminary. A critical evaluation of available research is warranted.
Adherence to these principles promotes a responsible and informed approach to the utilization of herbal infusions, maximizing potential benefits while mitigating potential risks.
The subsequent sections will explore potential risks and contraindications associated with specific plants, reinforcing the importance of a judicious and cautious approach.
1. Botanical Identification
Accurate botanical identification forms the cornerstone of safe and effective utilization of plant-derived infusions for allergy management. Misidentification can lead to the use of ineffective or even harmful plants, potentially exacerbating allergic symptoms or causing adverse reactions. The chemical composition of plants varies significantly, even within the same genus. Therefore, correct identification ensures the consumer receives the intended therapeutic compounds. For example, mistaking foxglove (Digitalis purpurea), a toxic plant, for comfrey (Symphytum officinale), sometimes used for its purported anti-inflammatory properties, could have severe consequences.
The importance of botanical identification extends beyond preventing acute toxicity. Different species and even subspecies of plants can have varying concentrations of active compounds. For instance, two cultivars of chamomile (Matricaria chamomilla) may possess differing levels of bisabolol, a compound believed to contribute to its anti-inflammatory and anti-allergenic properties. Consistent identification practices within the supply chain, from harvesting to processing, are necessary to guarantee the consistency and reliability of the final product. Third-party testing, utilizing methods like DNA barcoding or microscopic analysis, further validates botanical authenticity.
In summary, precise botanical identification is paramount to ensure the safety and efficacy of plant-based preparations intended for allergy relief. Neglecting this critical step can undermine the potential benefits and introduce significant risks. Robust quality control measures, including expert identification and analytical testing, are essential to guarantee the consumer receives a product that is both authentic and safe for consumption, thus facilitating responsible and informed utilization of botanical infusions.
2. Preparation Methods
Preparation methods significantly influence the efficacy and safety of plant-derived infusions used to manage allergic responses. The extraction of active compounds, the preservation of volatile oils, and the minimization of potential contaminants are all directly affected by the specific techniques employed.
- Water Temperature
Water temperature determines which compounds are extracted from the plant material. Overly high temperatures can degrade delicate volatile oils and heat-sensitive molecules, reducing the tea’s therapeutic potential. Conversely, insufficient heat may result in incomplete extraction of beneficial compounds. For example, chamomile requires a lower water temperature (around 170-180F) to preserve its calming constituents, while ginger may benefit from slightly higher temperatures to extract its pungent compounds effectively.
- Steeping Time
The duration of steeping impacts the concentration of active ingredients in the final infusion. Under-steeping may lead to a weak tea with limited therapeutic effect, whereas over-steeping can release bitter tannins and other undesirable compounds that detract from the flavor and potentially cause gastrointestinal distress. Optimal steeping times vary depending on the plant material. Leafy herbs generally require shorter steeping times (3-5 minutes), while roots and barks may need longer infusions (10-20 minutes) to fully release their beneficial components.
- Plant Material Preparation
The form of the plant material whether whole, cut and sifted, or powdered affects the rate and extent of compound extraction. Finely ground herbs have a larger surface area, allowing for faster extraction, but they may also release more sediment into the tea. Whole or coarsely cut herbs require longer steeping times but generally produce a cleaner cup. The choice of preparation method should align with the specific plant and the desired characteristics of the final infusion.
- Filtration and Storage
Proper filtration removes particulate matter and sediments from the infusion, improving its palatability and potentially reducing gastrointestinal irritation. Storage conditions, including exposure to light, air, and heat, can degrade the active compounds over time. Storing properly prepared infusions in airtight, dark-colored containers in a cool, dry place helps to preserve their potency and freshness.
These preparation methods are interrelated and critical for producing beneficial beverages. By understanding and applying these techniques correctly, individuals can maximize the potential benefits of these plants for supporting allergy management while minimizing the risk of adverse effects. A nuanced approach is key, considering the specific characteristics of each plant and tailoring the preparation method accordingly to optimize extraction and preservation of desirable constituents.
3. Symptom Relief
The purported benefits of plant-derived infusions in allergy management are primarily centered on symptom relief. Allergic reactions trigger a cascade of physiological responses, leading to various discomforts such as sneezing, itching, nasal congestion, and watery eyes. Certain plants contain compounds believed to modulate these responses, potentially mitigating the severity of symptoms. For example, quercetin, found in plants like onions and apples, is a bioflavonoid that exhibits antihistamine and anti-inflammatory properties. Individuals experiencing seasonal allergies might consume infusions containing quercetin-rich herbs, such as stinging nettle, with the intention of reducing histamine release and alleviating nasal congestion.
However, the efficacy of plant-derived infusions for symptom relief varies considerably depending on the specific plant, the individual’s physiological response, and the severity of the allergic reaction. Some plants, like chamomile, possess compounds with mild sedative effects, which may indirectly alleviate allergy symptoms by promoting relaxation and reducing stress. Others, such as ginger, contain anti-inflammatory compounds that may help to reduce swelling and irritation in the nasal passages. It is crucial to recognize that symptom relief achieved through plant-derived infusions is often subjective and may not provide complete resolution of allergic symptoms. Furthermore, the timing of consumption is essential; for example, individuals may start consuming these infusions before the onset of allergy season to build up a baseline of symptom management.
In conclusion, the connection between symptom relief and plant-derived infusions for allergy management lies in the potential of certain plants to modulate the physiological responses associated with allergic reactions. While anecdotal evidence and some preliminary research suggest that these infusions may provide symptomatic relief, it is essential to approach their use with caution and realistic expectations. Plant-derived infusions should not be considered a substitute for conventional medical treatments for allergies, but rather a complementary approach to managing symptoms and promoting overall well-being. Careful consideration of potential interactions, individual sensitivities, and the limitations of scientific evidence is paramount.
4. Potential Interactions
The consumption of plant-derived infusions for allergy relief warrants careful consideration of potential interactions with pharmaceutical medications and pre-existing health conditions. The bioactive compounds present in many plants can alter the absorption, metabolism, and excretion of drugs, leading to either reduced efficacy of prescribed treatments or increased risk of adverse effects. These interactions can occur through various mechanisms, including inhibition or induction of hepatic enzymes, competition for receptor binding sites, and alterations in gastrointestinal pH.
For instance, individuals taking anticoagulant medications, such as warfarin, should exercise caution when consuming infusions containing compounds like coumarin, which can potentiate the effects of the drug and increase the risk of bleeding. Similarly, certain plants may interact with immunosuppressant medications, affecting their efficacy in managing autoimmune conditions or preventing organ rejection. A pertinent example involves grapefruit juice, known to interact with numerous medications; while not an infusion itself, it illustrates the principle that compounds in plants can significantly alter drug metabolism. Moreover, individuals with underlying liver or kidney disease may be more susceptible to the adverse effects of plant-drug interactions due to impaired detoxification pathways. Failure to acknowledge potential interactions can result in serious health consequences, underscoring the need for open communication with healthcare providers.
In summary, the possibility of plant-drug interactions necessitates a cautious and informed approach to using infusions for allergy management. Healthcare professionals should be consulted to assess individual risk factors and potential contraindications. An understanding of these interactions is not merely academic; it is essential for ensuring patient safety and optimizing therapeutic outcomes. Awareness of these interactions facilitates a more responsible and effective integration of botanical preparations into overall allergy management strategies.
5. Quality Control
Stringent quality control is paramount in the production and distribution of plant-derived infusions intended for allergy management. Given the potential for variability in plant composition, contamination, and misidentification, a rigorous quality assurance program is essential to ensure product safety, efficacy, and consistency. These controls protect consumers from unintended adverse effects and promote informed decision-making regarding allergy relief strategies.
- Botanical Authentication
Accurate botanical identification is the first line of defense in quality control. Microscopic analysis, DNA barcoding, and chromatography are employed to verify the plant species used in the infusion. Absence of proper botanical authentication may lead to the inclusion of ineffective or harmful species. For example, adulteration of chamomile with other Asteraceae family members, some of which can cause allergic reactions, would negate any potential benefits and introduce a safety risk.
- Contaminant Testing
Plant-derived infusions are susceptible to contamination from various sources, including heavy metals, pesticides, molds, and bacteria. Quality control protocols must incorporate testing for these contaminants to ensure levels remain below established safety thresholds. Failure to conduct such testing can expose consumers to potentially toxic substances. A batch of nettle tea, for instance, could contain unsafe levels of lead if the plants were grown in contaminated soil.
- Active Compound Standardization
The concentration of active compounds responsible for the purported therapeutic effects can vary significantly among plant batches due to factors such as growing conditions, harvesting practices, and processing methods. Standardization involves quantifying the levels of key active compounds and ensuring that each batch meets a predetermined specification. Lack of standardization results in inconsistent product efficacy. For instance, if the rosmarinic acid content of a lemon balm infusion varies widely between batches, the expected antihistamine effect will be unpredictable.
- Stability Testing
Plant-derived infusions can degrade over time, leading to a loss of potency and the formation of potentially harmful degradation products. Stability testing involves monitoring the chemical composition of the infusion under various storage conditions to determine its shelf life and ensure that it remains safe and effective throughout its intended use. Without stability testing, a product might lose its therapeutic properties before its expiration date, rendering it ineffective for allergy symptom management.
These facets of quality control are interconnected and vital for ensuring the safety and efficacy of plant-derived infusions for allergy management. By adhering to stringent quality standards, manufacturers can provide consumers with reliable products that meet their expectations and promote informed decision-making regarding their health. Neglecting any of these aspects compromises the integrity of the product and introduces unnecessary risks.
6. Long-term Use
The extended consumption of plant-derived infusions for allergy management introduces a complex interplay of potential benefits and risks. Continuous exposure to the bioactive compounds present in these infusions can lead to cumulative effects on various physiological systems. Understanding these long-term implications is crucial for responsible integration of these beverages into a wellness regimen. For example, consistent consumption of licorice root infusions, while potentially beneficial for adrenal support, can elevate blood pressure in susceptible individuals over time, necessitating careful monitoring.
Furthermore, the long-term use of certain plant-derived infusions may impact the gut microbiome, influencing both immune function and overall health. Specific plants possess prebiotic properties, fostering the growth of beneficial bacteria, while others may exert antimicrobial effects, potentially disrupting the balance of the gut ecosystem. These alterations, in turn, may modulate the body’s response to allergens, either enhancing or diminishing the intended therapeutic effects. Consistent monitoring and awareness of these potential shifts becomes vital when considering extended consumption.
In summary, the long-term utilization of plant-based infusions for allergy support presents a nuanced picture. While some individuals may experience sustained symptomatic relief and improved well-being, it is essential to acknowledge the potential for cumulative effects and to remain vigilant for any adverse reactions. Healthcare professionals should be consulted to assess individual suitability and to monitor for potential long-term consequences, thereby ensuring safe and responsible integration of these infusions into allergy management strategies.
Frequently Asked Questions
The following addresses common inquiries and misconceptions surrounding the use of botanical infusions as a complementary approach to managing allergic conditions. Information provided is intended for educational purposes and does not constitute medical advice.
Question 1: Are plant-derived infusions a substitute for conventional allergy medications?
Plant-derived infusions should not be regarded as replacements for prescribed allergy medications. While certain botanicals may offer symptomatic relief, they do not address the underlying immunological mechanisms of allergic reactions in the same manner as pharmaceutical interventions. These infusions should be considered a complementary approach, used in conjunction with, and not in lieu of, conventional treatments prescribed by a healthcare professional.
Question 2: How quickly can one expect to experience allergy relief from botanical infusions?
The onset of symptom relief from plant-derived infusions varies significantly based on individual physiology, the specific plant used, the severity of the allergic reaction, and consistency of consumption. Unlike fast-acting antihistamines, the effects of these infusions may be gradual, requiring consistent, long-term integration into a daily routine to observe noticeable benefits. A realistic timeframe for assessing efficacy may range from several weeks to months.
Question 3: Are all plant-derived infusions safe for consumption during pregnancy or breastfeeding?
Not all botanical infusions are safe for consumption during pregnancy or breastfeeding. Certain plants contain compounds that may pose risks to fetal development or infant health. Prior to incorporating any plant-derived infusion into the diet during these periods, consultation with a qualified healthcare provider or herbalist is essential to assess potential risks and benefits.
Question 4: How can one ensure the quality and purity of plant-derived infusions?
Ensuring quality and purity requires selecting reputable suppliers known for rigorous quality control measures. Look for products that have undergone third-party testing for botanical identification, heavy metals, pesticides, and other contaminants. Reading product labels carefully and researching the manufacturer’s sourcing and production practices is also essential.
Question 5: Can plant-derived infusions interact with other medications?
Yes, plant-derived infusions can interact with various pharmaceutical medications, altering their absorption, metabolism, or excretion. Individuals taking prescription or over-the-counter medications should consult with a healthcare professional before consuming botanical infusions to assess potential interactions and avoid adverse effects.
Question 6: What are the potential side effects associated with long-term consumption of plant-derived infusions?
Long-term consumption of plant-derived infusions may be associated with various side effects, depending on the specific plant and individual susceptibility. Some plants can affect blood pressure, liver function, or hormone levels. Ongoing monitoring by a healthcare professional is advisable to detect and manage any potential adverse effects.
The responsible and informed utilization of plant-derived infusions necessitates a comprehensive understanding of their potential benefits, risks, and limitations. Consultation with qualified healthcare professionals is paramount.
The following section will provide resources for further exploration of the topic, encouraging continued learning and informed decision-making.
Conclusion
This exploration has illuminated the complexities surrounding the use of herbal teas for allergies. Key aspects, from botanical identification and preparation methods to potential interactions and long-term effects, necessitate careful consideration. While anecdotal evidence and some research suggest potential benefits for symptom relief, these preparations are not a substitute for conventional medical treatments. The importance of quality control, accurate identification, and consultation with healthcare professionals cannot be overstated.
The responsible integration of these botanical infusions into allergy management demands a balanced perspective, weighing potential advantages against inherent risks. Future research is warranted to further elucidate the efficacy and safety profiles of specific plant-derived infusions. The informed consumer, guided by scientific evidence and professional medical advice, is best positioned to navigate the nuanced landscape of herbal teas for allergies.